In September 2020, the AARP Public Policy Institute released its fourth Long-Term Services and Supports (LTSS) State Scorecard, Advancing Action: A State Scorecard on Long-Term Services and Supports for Older Adults, People with Physical Disabilities, and Family Caregivers. Funded by The SCAN Foundation and The Commonwealth Fund, the LTSS State Scorecard showcases state performance for creating a high-quality system of care.
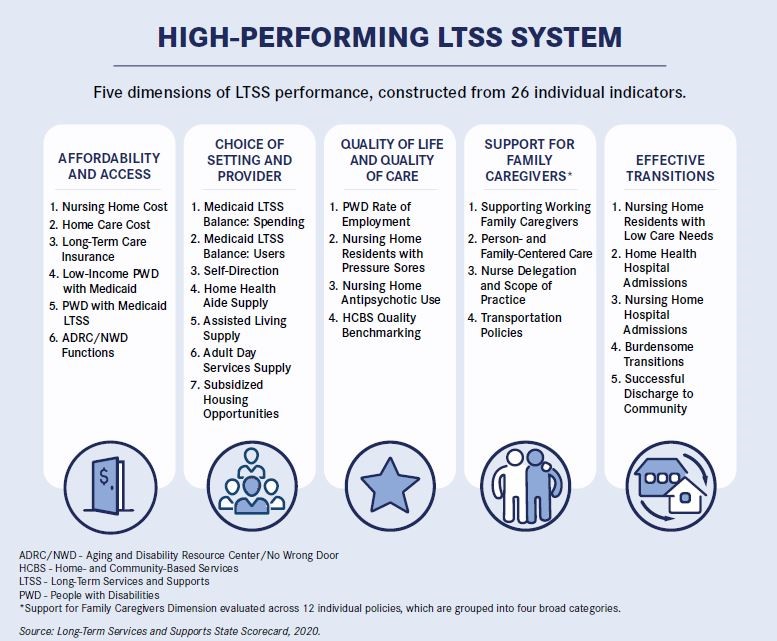
First released in 2011, the Scorecard provides comparable data for state leaders, stakeholders and providers to benchmark performance, measure progress and identify key areas of improvement. The 2020 Scorecard evaluated LTSS performance across five dimensions, through 26 indicators.
Scorecard in a Time of COVID-19
Released in the midst of a global pandemic, the 2020 LTSS State Scorecard reflects state performance prior to COVID-19. The pandemic has brought increased focus on the state’s LTSS system, revealing challenges and opportunities for reshaping how services are delivered and financed. Federal response to the pandemic has allowed states new flexibilities to provide LTSS in ways that may create lasting delivery system change.
With COVID-19 came new care experiences and fast-tracking of others already in existence (e.g., telehealth). Some innovations have not only increased access to home- and community-based services (HCBS), but also illuminated previously hidden barriers. Measures in the 2020 LTSS Scorecard provide a useful framework for understanding state performance in a pre-COVID era and planning for LTSS improvements.
Key Findings Across States
Millions of Americans will face greater health needs over the next few decades, and this Scorecard shows that we are still falling short of where we need to be to address those needs. States have made some progress since 2017 to improve care options, but not enough to keep up with demographic demands. In fact, of the 21 measures looking at performance over time, more than 30 states remained stagnant—showing little or no improvement in 15 measurement areas. Additionally, more than 20 states saw a significant decline in the number long-term care insurance policies issued, which is concerning considering that more than half of people turning age 65 will have an LTSS need at some point.
Beyond this stagnation, there are five areas in which more than 20 states showed significant improvement.
- Person and Family-Centered Care: This indicator measures performance in three policy areas: Medicaid spousal impoverishment protections; family caregiver needs assessment; and enactment of the Caregiver Advise, Record, Enable (CARE) Act. Scorecard findings show that 29 states showed significant improvement, with the biggest driver being states implementing family caregiver assessments.
- Supporting Working Family Caregivers: Family caregivers continue to play a vital role in the well-being of millions of people. Recognizing this, more states are enacting policies that support working family caregivers. Scorecard results show more than a third of states have state or local laws mandating paid sick days for family caregivers. Additionally, more states and localities now allow employees to use accrued sick time for purposes other than their own illness; and nine states have enacted paid family leave.
- Aging and Disability Resource Center (ADRC) Functions/No Wrong Door System: In many states, LTSS systems are fragmented and difficult for people to navigate, creating barriers to accessing services that could improve quality of life and reduce the strain on family caregivers. Over the years, states have created ADRCs as a single place for people to learn about and access LTSS. These ADRCs differ significantly across states in the services and supports that they offer. The Scorecard shows that 33 states demonstrated significant improvement by expanding ADRC functions and capabilities to better serve older adults, people with disabilities and family caregivers.
- Improving the Medicaid LTSS Spending to Better Balance Dollars Spent on HCBS vs. Institutional Care: Most people want to remain in their homes and communities as they grow older. States that strike the right balance in Medicaid funding between nursing homes and HCBS help individuals with lower incomes meet this goal. Since the last Scorecard, half of states improved spending on HCBS.
- Nursing Home Antipsychotic Medication Usage: Historically, nursing homes have been known to use antipsychotic medications inappropriately to manage behaviors, instead of using more person-centered, less invasive measures. The 2020 State Scorecard reflects a promising trend with continued decline of inappropriate use of antipsychotic medications in nursing homes. That said, more research is needed to determine how this decrease in inappropriate usage has been accomplished (e.g., increased frequency in schizophrenia diagnoses, staff ratios, training).
All states, even those that performed well, still have work to do. And, the heightened attention on LTSS due to COVID-19 has only exposed system inadequacies that, across the years, the Scorecard has brought to light. At a time when states may shy away from LTSS system improvements due to budgetary challenges, there are ways to leverage the public and private sectors to create efficient and affordable system improvements.Ideally, all states would have high-performing LTSS systems in which older adults, people with disabilities and family caregivers have access to high-quality, affordable choices that address their needs. Looking forward, the 2020 LTSS State Scorecard can be used to identify priorities and mechanisms to advance action for LTSS system improvements through the COVID-19 pandemic and beyond.
Megan Burke, LCSW, is a policy analyst at The SCAN Foundation in Long Beach, Calif.













