The rising older population and evolution of technology is prompting many elder care communities to adapt to the changing needs of residents. Today, newer buildings feature restaurants, fitness centers and dedicated entertainment spaces, as well as additional communal spaces to foster social connections.
From an infrastructure perspective, many of these buildings have been upgraded to include assistive technologies and telehealth capabilities, as well as adaptable spaces to support different levels of care as residents age or have acute care needs. Now, the rise of AI has the potential to further improve the resident experience and staff management with the goal of designing even safer communities.
The Importance of Quality Data to Support AI
While the field of AI has been around for decades, the widespread use of it is relatively new. As it evolves, it has the potential to change how we live and work. From the perspective of a long-term care community, AI is being used in a variety of ways. These include robotics for mobility assistance, medication management, fall detection, and earlier identification of subtle changes in movement that may signal yet undetected health issues.
Underlying all these AI-driven innovations is data. Without accurate data, AI models can’t be properly trained to perform as expected. For example, several instances of AI generating false information have made their way into the mainstream media. This doesn’t mean AI can’t work, it simply means that the underlying data required to train the models is faulty.
How AI-Driven Data Boosts Safety
When it comes to elder care communities, before AI can deliver any benefits, one needs to understand how buildings are used by residents and staff. While there may be dedicated areas for dining, physical therapy, and socializing; one cannot make assumptions about how the space is actually used.
‘AI-driven data may provide fresh insight that Saturday early evening in the dining area is a more popular time.’
For example, it may be assumed that most family visits happen in the common area on Sunday afternoons. Yet AI-driven data may provide fresh insight that Saturday early evening in the dining area is a more popular time. Based on this data, staffing schedules might be rethought, and the dining area layout could be designed to be more ergonomic.
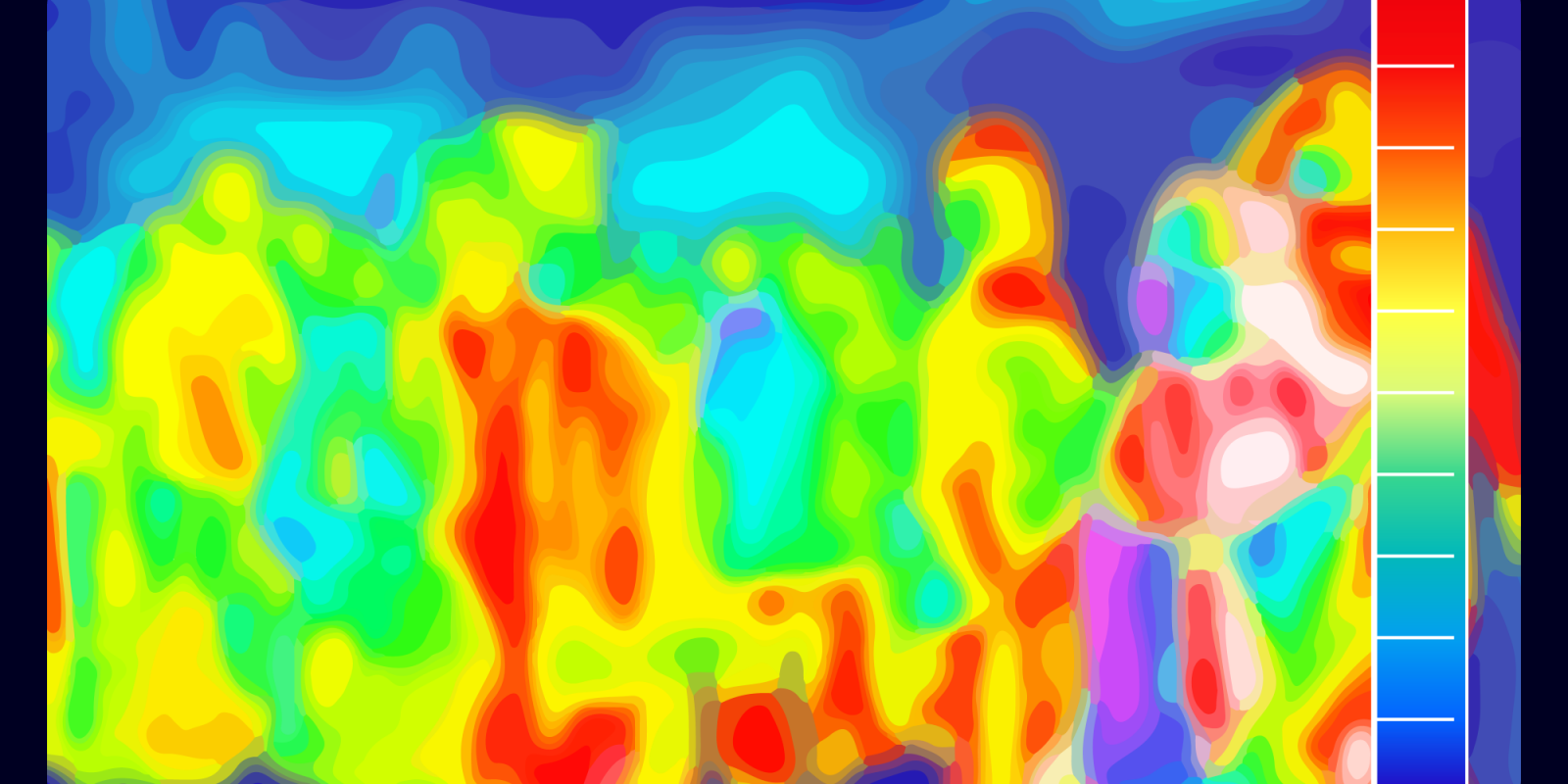
AI provides this insight by fusing with body-heat-sensing technology to understand subtle human movements, including gait speed and activity. By installing private, wireless sensors on the wall, the AI infers activity yet ensures 100% anonymity. The sensors are built to understand how humans interact in a space and display these actions as infrared “heat blobs,” yet do not need to know which individuals were present in order to provide insight.
Another example is the use of AI to differentiate between a UTI and dementia. This misdiagnosis is common because UTIs can cause delirium in older adults, which presents similarly to dementia. However, having insight into subtle changes in behavior such as frequency of bathroom visits can help make a diagnosis more quickly and more accurately. Conversely, it can also provide insight such as a rise in a resident’s wandering incidents, which may signal worsening cognitive decline.
These data points offer tremendous insight and the ability to get ahead of potential health issues. They also can be shared and paired with other data sources used by the elder care community’s administrators, physicians or healthcare providers to give residents optimal care.
Back to the wandering incident, one can also set alerts to these types of actions, enabling staff to respond more quickly. And, during shifts when staff may be stretched thin, AI can support passive check-ins without compromising care or risking safety. This is especially valuable during night shifts because it helps staff and managers focus on needs-based care, as opposed to time-driven rounds.
These examples show how AI and data can establish benchmarks that provide care administrators with trend data that can be used to make strategic decisions about residents and buildings.
Ensuring Privacy
Of course, privacy remains one of the biggest concerns when it comes to AI, especially in elder care communities. Many technologies aim to provide privacy and safety, yet can be cumbersome (wristbands, for example), or require additional resources to set up and manage. For these reasons, when evaluating AI for use in buildings, be sure to ask about:
- Privacy: for resident activity and any building-related data,
- Upfront and ongoing costs for acquiring, installing, and managing the technology,
- Potential downtime: of private rooms or common areas while the technology is being installed.
As the demand for long-term care communities grows, AI can play a vital role in delivering higher quality resident experiences.
Honghao Deng is the CEO and co-founder of Butlr in San Francisco.
For more on AI as it relates to older adults, watch for our Summer 2025 issue of Generations journal.
Illustration caption: Heat sensor technology at work.
Illustration credit: Shutterstock/cipta studio