Alzheimer’s disease and related dementias (ADRD) represent significant public health challenges globally that affect the quality of life and independence of millions of older adults, their families and healthcare systems. According to a recent World Health Organization report, approximately 57 million people had dementia worldwide, with global costs related to dementia estimated at $1.3 trillion. In the United States, an estimated 7.2 million Americans are living with Alzheimer’s dementia, with total medical and long-term care expenditures for those ages 65 and older with ADRD projected to reach $384 billion. Due to rapid population aging in the United States and worldwide, the number of older adults with dementia is projected to increase substantially over the coming decades.
Despite these demographic projections, there is growing evidence from studies in the United States and other high-income countries that suggests the prevalence and incidence of ADRD are declining, and the average age at which ADRD is diagnosed is increasing, resulting in older adults, on average, spending a greater number of their late-life years cognitively healthy. These encouraging trends suggest that greater educational attainment, better management of chronic diseases such as diabetes and hypertension, and reduced rates of smoking have had positive population-level effects regarding ADRD.
In the United States, population aging has coincided with growing racial and ethnic diversity. Recent population projections from the U.S. Census Bureau, illustrated in Figure 1, below, indicate that racial and ethnic minority groups ages 65 and older are expected to experience the highest rates of population growth.
Figure 1: Projected Population Distribution of Adults 65 and Older by Race and Ethnicity
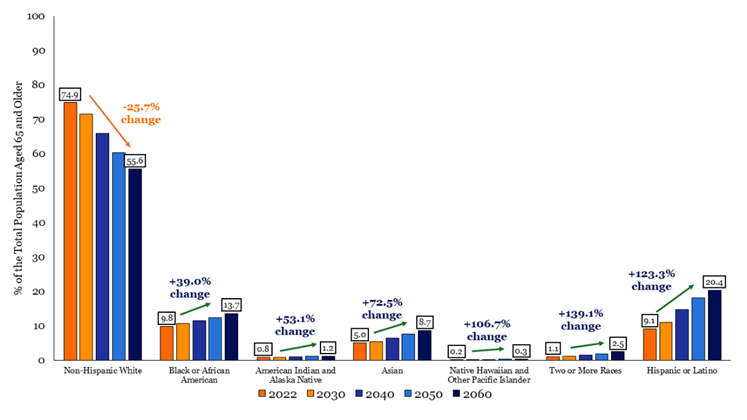
Data Source: U.S. Census Bureau, Population Division. (2023). Projected Population Distribution by Race, Hispanic Origin, and Selected Age Groups for the United States, Main Series: 2022–2060.
Notably, these groups are more likely than their white counterparts to experience greater lifetime exposure to socioeconomic disadvantage (e.g., income inequality, barriers to education, and unequal access to quality healthcare), which increases the risk of health conditions such as hypertension and diabetes that are risk factors for dementia. Many of the above minority groups are also projected to have the highest prevalence of Alzheimer’s dementia in the coming years.
Measuring Population Health
Cognitive healthy life expectancies are defined as the number of remaining years, at a particular age, that an individual can expect to live in a cognitively healthy state. This population metric combines mortality rates with the prevalence of different cognitive states (i.e., normal cognition, cognitive impairment/no dementia, and dementia) to provide a more nuanced picture of population health than total life expectancy or dementia prevalence alone. Researchers and policymakers have widely used this population surveillance tool to measure the cognitive health of a population and promote cognitive health among older populations, enabling individuals to remain active and productive in the economy for longer.
‘Cognitive healthy life expectancies are defined as the number of remaining years, at a particular age, that an individual can expect to live in a cognitively healthy state.’
Figure 2, below, illustrates cognitive life expectancy estimates based on data from the Health and Retirement Study (HRS). There are two main findings: 1) Higher educational attainment among older adults is associated with an increase in both the number of years lived cognitively intact and the proportion of late-life years after age 65 lived cognitively healthy, regardless of other demographics; 2) Despite similar levels of educational attainment, stark racial/ethnic and nativity disparities in cognitive health life expectancies at age 65 are evident, with older white adults, regardless of sex, living a greater proportion of their remaining lives cognitively healthy than older minority adults.
Figure 2: Cognitive Health Life Expectancies by Race/Ethnicity, Sex, and Educational Attainment.
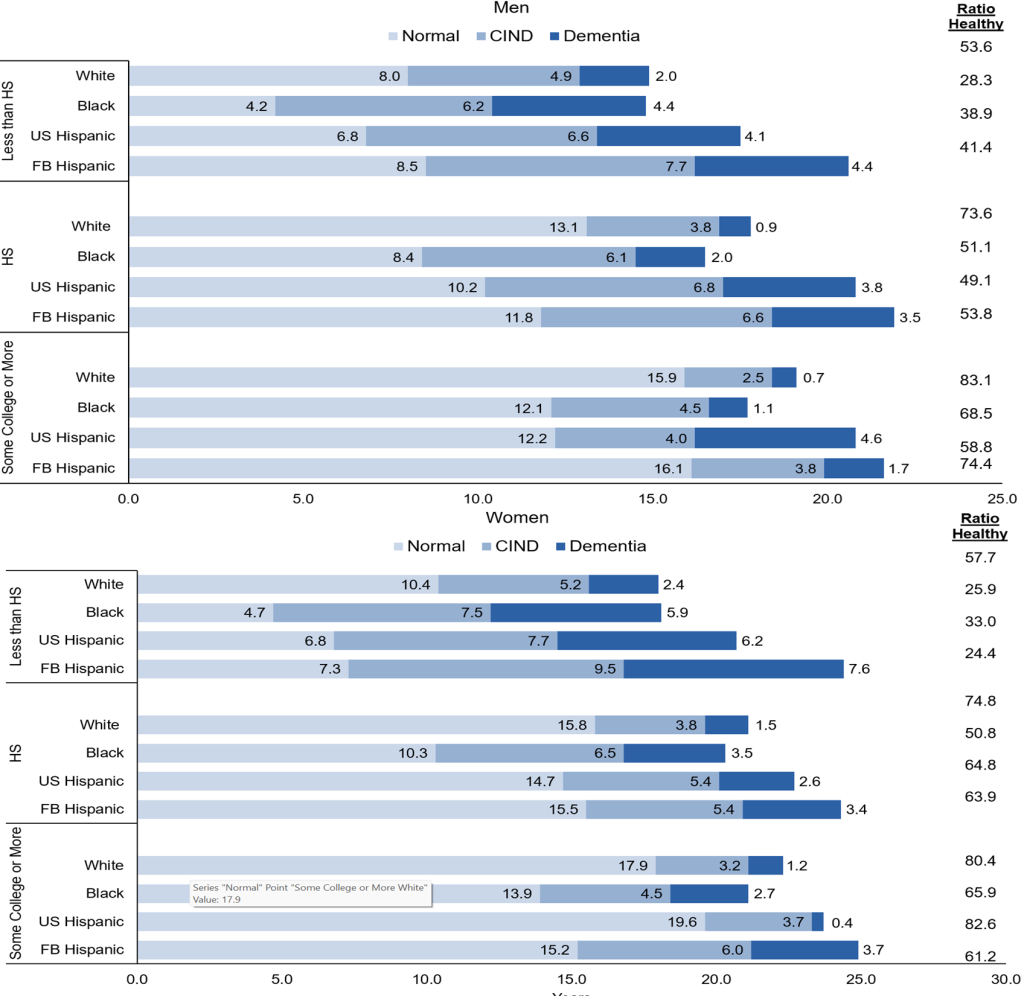
Data Source: Health and Retirement Study. Garcia, M. A., Downer, B., Chiu, C. T., Saenz, J. L., Ortiz, K., & Wong, R. (2021). Educational benefits and cognitive health life expectancies: Racial/ethnic, nativity, and gender disparities. The Gerontologist, 61(3), 330–340.
While all Americans have experienced increasing educational attainment over recent decades, persistent racial/ethnic disparities remain. Racial/ethnic disparities in cognitive health outcomes in the United States have been attributed in part to long-standing and deeply rooted inequalities in educational attainment and quality of education. Thus, the above results, coupled with projected demographic changes, highlight the need for programs focused on increasing educational attainment and quality of education, particularly for women and minority populations, to create better equity and improved social and economic outcomes that lead to cognitively healthier lives.
Notably, greater educational attainment is also associated with lower risk for other important risk factors associated with poor cognitive functioning, such as chronic health conditions, better health behaviors, and higher socioeconomic status. Moreover, higher educational attainment in young adulthood can lead to higher occupational status, better healthcare access, and better opportunities to engage in mentally and physically stimulating activities, which can be beneficial for cognitive functioning and staying active in the economy later in life.
Notably, greater educational attainment is associated with lower risk for other important risk factors associated with poor cognitive functioning.
While there is currently no known cure, continued public health efforts aimed at addressing ADRD health disparities, creating more responsive healthcare systems for those impacted by ADRD, and enhancing the quality of life for affected individuals and their caregivers can benefit the economy by increasing workforce participation, reducing healthcare spending, and boosting productivity.
Programs that increase overall education and ADRD health literacy have the potential to improve adherence to lifestyle changes (e.g., exercise and smoking cessation) and other health recommendations (e.g., improved diabetes management) aimed at reducing vascular risk factors associated with accelerated brain aging. Such programs, if designed with input from relevant stakeholders, may significantly lessen the healthcare and caregiving burdens related to ADRD by helping individuals remain active in the economy longer.
These programs may also potentially lessen the cognitive health inequalities for future cohorts of older adults in the United States. Given the growth of minority populations in the United States, research and public policy efforts should be directed to the development and implementation of programs aimed at promoting brain health to ensure all older adults have an equal opportunity to maintain their cognitive function across the lifespan.
Marc A. Garcia, PhD, is an associate professor in the Department of Sociology and a Research Associate of the Aging Studies Institute in the Maxwell School at Syracuse University, Syracuse, New York.
Photo credit: Shutterstock/Vitalii Vodolazskyi













