Gallup and West Health have unveiled a new, first-of-its-kind state-by-state ranking measuring how Americans experience the healthcare system, not through claims or spending totals, but through their lived experience. The new West Health-Gallup Center on Healthcare in America offers an unprecedented look at healthcare cost, access and quality across all 50 states and Washington, DC. It brings clarity to a system where residents in one state may face high treatment costs or limited appointment availability, while others experience reliable access and consistent, high-quality care.
While the rankings encompass all adults, two groups stand out: older adults ages 65 and older, many of whom rely upon Medicare, and adults ages 50–64, a demographic often managing more chronic conditions while still in the workforce and not yet eligible for full Medicare benefits. A closer look at the State of the States 2025 data reveals important differences and shared challenges between these two populations.
Healthcare Affordability: Persistent Pressures for Older Adults
Among adults ages 65 and older—who are more likely to be insured through Medicare—affordability remains a significant concern. Nationally, for adults ages 65 and older:
- 40% experience “a lot” or “some” stress related to healthcare costs.
- 15% report healthcare costs are a “major” financial burden.
- 13% say they or someone in their family skipped prescribed medication in the past year to save money.
- 11% avoided doctor-recommended tests or treatments because they could not afford them.
These findings challenge the assumption that Medicare universally protects older adults from cost barriers. Despite broad coverage, Medicare still leaves significant gaps, with many older adults facing high out-of-pocket costs for prescription drugs, diagnostics and specialist care. Note that we cannot distinguish between respondents who have Traditional Medicare vs. Medicare Advantage or other supplemental coverage.
For adults ages 50–64, healthcare affordability challenges are even more pronounced—reflecting rising deductibles, variability in employer coverage, and insurance churn. Among this group:
- 53% experience “a lot” or “some” stress related to healthcare costs.
- 24% report healthcare costs as a “major” financial burden—nearly 10 percentage points higher than adults ages 65 and older.
- 22% say they or someone in their family skipped prescribed medication in the past year to save money —almost double the rate among adults ages 65 and older.
- 30% avoided doctor-recommended tests or treatments because they could not afford them—nearly triple the rate among adults ages 65 and older.
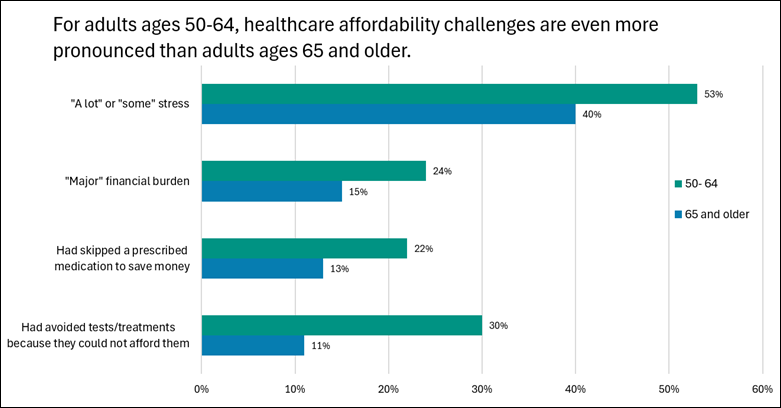
These stark differences underscore a system in which adults nearing retirement age, often managing chronic conditions, face some of the most substantial affordability pressures.
More than half (53%) of older adults ages 50–64 and 40% of adults ages 65 and older report that they experience some or a lot of stress related to healthcare costs.
Healthcare Access: Challenges Remain for Older Adults
Difficulties accessing care affect both groups, though adults ages 50–64 encounter more obstacles than adults ages 65 and older. Nationally:
- 14% of adults ages 65 and older say it is “somewhat” or “very” difficult to access the healthcare services they need for physical health needs
- For adults ages 50–64, these access challenges rise to 19%.
These difficulties stem from issues such as long wait times for appointments, transportation limitations, geographic provider shortages, and fractured scheduling systems. While Medicare coverage helps stabilize access for older adults, those ages 50–64 often face a patchwork of insurance options, high provider network variability, and narrower access to specialists and mental health providers.
Healthcare Quality: A Stronger Area for Both
Across both age groups, perceptions of the quality of care they receive remain a bright spot.
Among adults ages 65 and older:
- 81% “strongly agree” or “agree” that their medical professionals provide high-quality care.
Among adults ages 50–64:
- 74% “strongly agree” or “agree” that their medical professionals provide high-quality care, slightly lower than in the ages 65 and older population.
These ratings reflect the stability of provider relationships and continuity of care, particularly as people get older.
Why These Numbers Matter
For policymakers, advocates and journalists, incorporating age-specific insights is essential. Adults ages 65 and older are the fastest-growing segment of the population, and those ages 50–64 will soon transition into Medicare, carrying their current affordability and access challenges with them. Understanding the distinct needs, barriers and care-seeking patterns of these age groups allows policymakers to anticipate pressure points in the healthcare system before they intensify. By grounding decisions in data that reflect the real experiences of older adults, policymakers are better equipped to craft interventions that strengthen Medicare’s long-term sustainability and improve how Americans experience the healthcare system as they age.
Explore the Data
These early findings only scratch the surface of what the new West Health-Gallup Center on Healthcare in America platform offers. The website allows users to compare states across dozens of indicators, examine strengths and weaknesses, and explore where Americans face the steepest challenges. Users can filter indicators by gender, age, race, income and more to see how different subpopulations experience healthcare. The site also includes long-term trends that track public opinion over the past two decades and show how care has changed over time, with testimonials that uncover the human side behind the numbers.
For more information on the methodology, click here.
Amy Herr, MHS, PMP, is senior director of Health Policy, and Niamh Brennan, MPH, is a research associate for the nonprofit, nonpartisan West Health Policy Center. Marissa Myers, MPP, is a research analyst for the nonprofit, nonpartisan West Health Institute.
Photo credit: Shutterstock/KAMONRAT













