As the American population ages, there is a greater need for compassionate care for all, especially the most vulnerable. Compounding this, almost 90% of American adults have been exposed to at least one traumatic event during their lifetime. Additionally, studies have shown that Holocaust survivors, racial and ethnic minoritized groups, LGBTQ+ individuals, immigrants and refugees, survivors of crime, survivors of disasters, individuals in “high-risk professions” (emergency responders, firefighters, police officers, etc.), veterans, and individuals with disabilities have high rates of trauma exposure.
The person-centered, trauma-informed (PCTI) approach is a holistic model of care that allows more effective care across the aging services sector. The PCTI approach promotes the health and well-being of individuals by recognizing the role of trauma across the life course, resisting retraumatization, and promoting the strength, agency, and dignity of people receiving care. While the PCTI approach has emerged as the gold standard to account for trauma in aging services and to support all aging populations, the aging sector’s capacity to use the PCTI approach remains unclear.
To better understand the use of the PCTI approach in the aging services sector, the Center on Aging, Trauma, and Holocaust Survivor Care (Center) published the 2026 National Study on the Person-Centered, Trauma-Informed (PCTI) Approach in Aging Services. The study comprises a sample of 274 organizations across the United States that range in sector, size, geographic location, religious affiliation, and service type. Its findings illuminated the state of PCTI care implementation across the aging services sector. The findings also include multiple gaps within the sector, highlighting barriers to PCTI care. Visit the following links to read the full report, executive summary, and infographic.
Awareness and Capacity of Aging, Trauma and the PCTI Approach
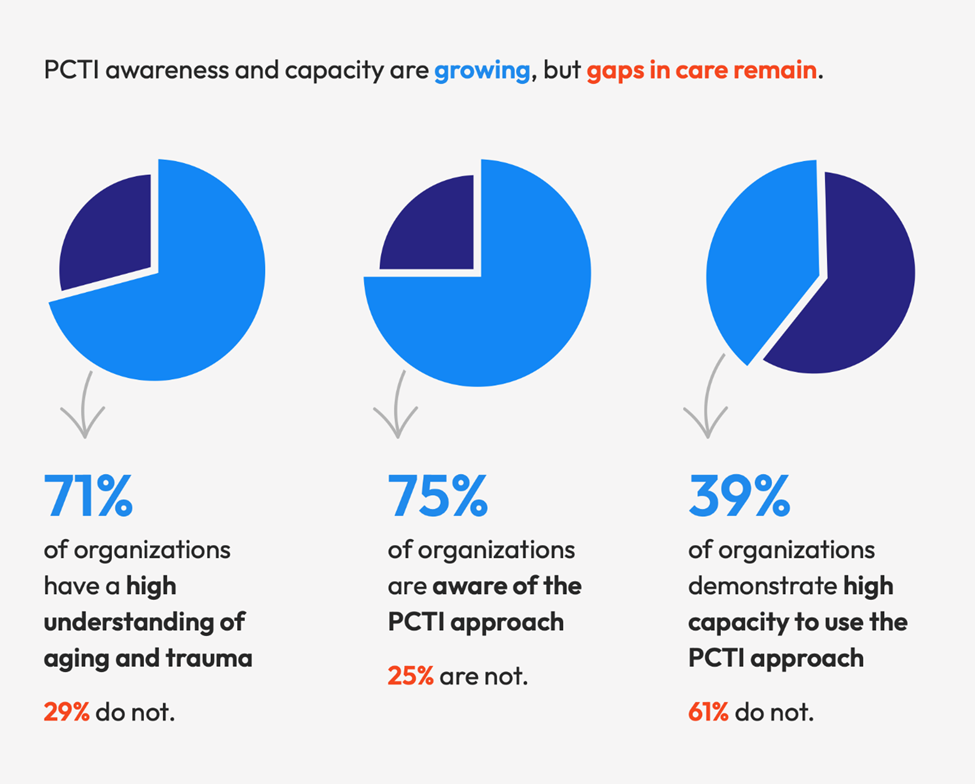
While most organizations reported awareness of the PCTI approach, awareness does not necessarily translate to understanding or capacity. Only a fraction of organizations that were aware of the PCTI approach demonstrated deep capacity to use the approach. Even more surprisingly, only 71% of surveyed organizations reported a high understanding of how trauma impacts aging (see Figure 1, below).
Figure 1. Findings on Aging, Trauma and the PCTI Approach
As the needs of the older population continue to increase, the direct care workforce must adapt to effectively serve older adults. This cohort’s changing needs will require more time, capacity, and knowledge from an already understaffed workforce. At the same time, direct care workers are experiencing high levels of burnout and secondary trauma as they attempt to address longstanding, sector-wide gaps in aging services. In response, aging services organizations must take an active role to support the direct care workforce while simultaneously implementing systems-level changes that promote workforce sustainability and well-being, as well as high quality PCTI care.
Care Across Populations
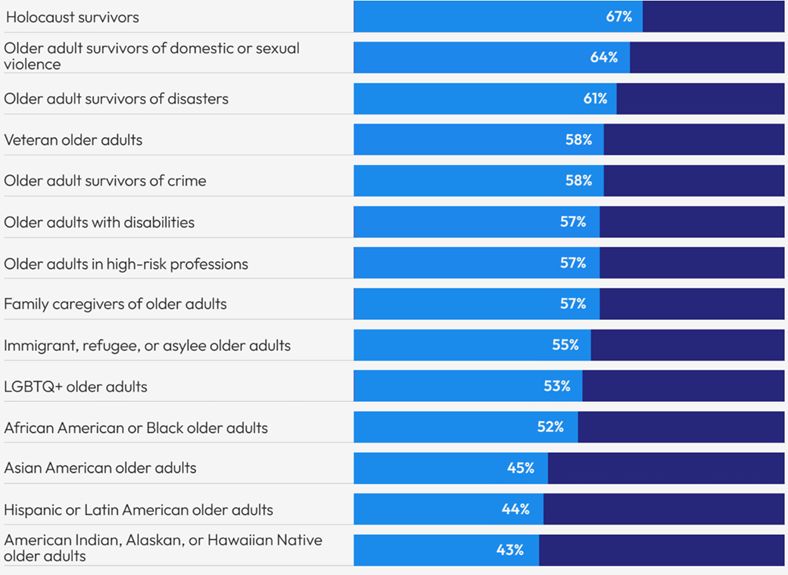
The report demonstrates that aging services providers have varying capacity to provide PCTI services across aging populations, resulting in higher or lower access to PCTI services based on service recipient identity. Organizations surveyed reported the lowest capacity to provide PCTI services to American Indian, Alaskan or Hawaiian Native older adults, Hispanic or Latin American older adults, and Asian American older adults. The highest capacity to provide PCTI services was to Holocaust survivors, older adult survivors of domestic or sexual abuse, and older adult survivors of disasters (see Figure 2, below).
Figure 2. Self-Reported PCTI Capacity Across Service Populations
Benefits of the PCTI Approach
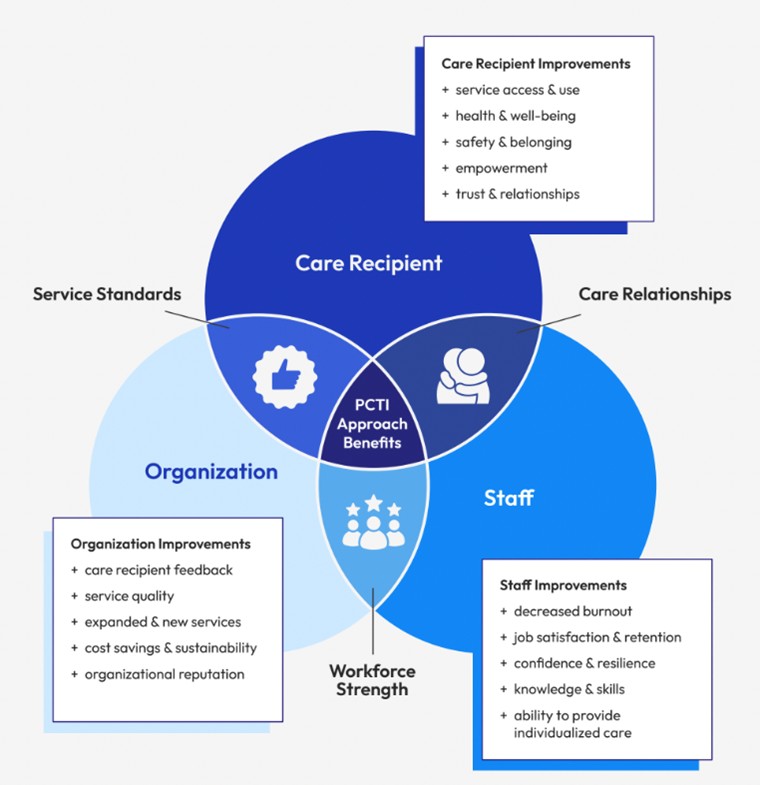
While there are gaps in PCTI care, organizations overwhelmingly see the benefits of using the approach. The PCTI approach is universal and can be used by anyone for anyone—including clients, staff, and organizations. Eighty-nine percent of surveyed organizations reported that the PCTI approach brings benefits to care recipients, staff, and their organization. When successfully implemented, there are benefits for everyone involved in care delivery (see Figure 3, below).
Figure 3. Benefits of the PCTI Approach
Call to Action
If you want to help promote person-centered, trauma-informed care for all older adults, here are some ways to start.
- Improve understanding about aging with a history of trauma. Enhance recognition and understanding of how trauma impacts older adults, their family caregivers, and the services provided.
- Increase understanding and application of the PCTI approach. Improve aging services professionals’ knowledge of the PCTI approach and its application, and train and coach colleagues to do the same.
- Build organizational capacity to use the PCTI approach. Dedicate time and resources to infuse the PCTI approach throughout an organization and its programming to provide compassionate care to all older adults and their family caregivers.
- Acknowledge PCTI care across populations. Learn about care across older populations and improve services to provide PCTI care to all older adults with a history of trauma and their family caregivers.
With these recommendations, you can infuse PCTI considerations throughout your work and improve the care that older adults and their family caregivers receive. When care is provided in a PCTI way, older Americans can age with safety, dignity, and compassion.
To learn more, visit www.AgingandTrauma.org and read “Compassionate Care in America: Results from the National Study on the Person-Centered, Trauma-Informed Approach.”
This work is supported by the Administration for Community Living (ACL), the United States Department of Health and Human Services (HHS) as part of a financial assistance award totaling $8,389,500 with 75% funded by ACL/HHS and $2,796,500 and 25% funded by non-government source(s). The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by ACL/HHS, or the United States Government.
Vanessa Rubenstein, MPH is Manager, Research and Evaluation, in the Center on Aging, Trauma, and Holocaust Survivor Care at Jewish Federations of North America in New York City.
Photo credit: wavebreakmedia













