Abstract
The Age-Friendly Health Systems movement, led by The John A. Hartford Foundation and the Institute for Healthcare Improvement, in partnership with many organizations and health systems, aims to address the growth of the older adult population and the challenges facing this population through the 4Ms framework: What Matters, Medication, Mentation, and Mobility. The 4Ms have been successfully integrated in various health systems, demonstrating improved care and positive outcomes. For long-lasting improvements to the health and care of all older adults, health systems need to collaborate with partners across the Age-Friendly Ecosystem.
Key Words
Age-Friendly Health Systems, age-friendly care, cross-sector collaboration, older adults, health equity
As we age, our healthcare needs can become more complex and health systems are frequently unprepared to meet them, resulting in older adults suffering disproportionate harm. This harm can be compounded by race, gender, sexual orientation, geography, and other factors, especially when an older adult embodies multiple identities. Older adults from historically marginalized communities suffer from disparate treatment that negatively influences health outcomes.
Age-Friendly Health Systems Overview
To address the impact of older adults on the healthcare system, in 2017 The John A. Hartford Foundation (JAHF) and the Institute for Healthcare Improvement (IHI), in partnership with the American Hospital Association (AHA) and the Catholic Health Association of the United States (CHA), set a bold vision to build a social movement so that all care with older adults is age-friendly care. In the Age-Friendly Health System’s movement, age-friendly care follows an essential set of evidence-based practices, known as the 4Ms (What Matters, Medication, Mentation, and Mobility); causes no harm; and aligns with What Matters to the older adult and their caregivers. When implemented together, the 4Ms represent a broad shift by health systems to focus on the needs of older adults (see Figure 1, below).
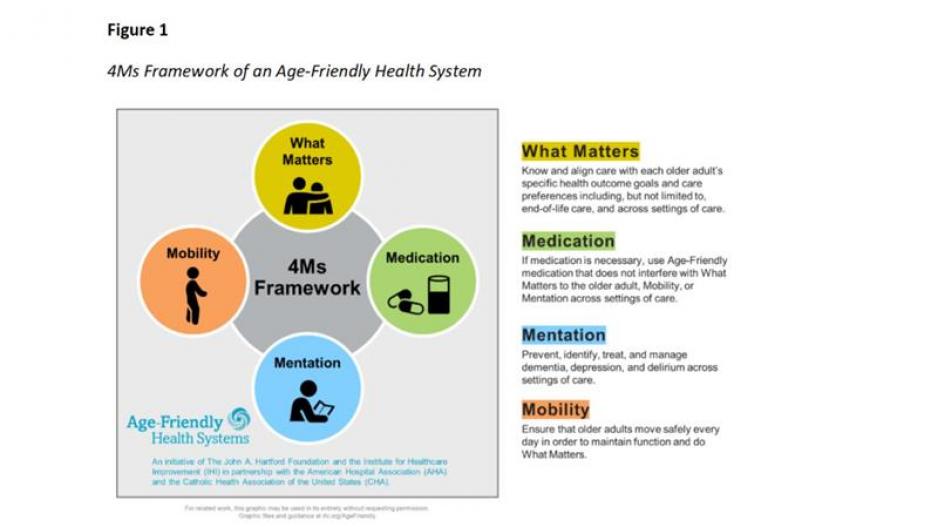
The 4Ms identify core issues that should drive decision-making in older adult care. They organize care, focus on the older adult’s strengths, and are relevant regardless of an older adult’s health status, conditions, or demographics (cultural, racial, ethnic, or religious background, or socioeconomic status). Care is structured and informed by What Matters most, while the 4Ms reinforce one another as a set (Tinetti, 2019).
Shifting the Culture of Care
The 4Ms are a framework, not a program, to guide care of older adults in every interaction with the healthcare system. The framework was developed after reviewing 17 care models and selecting the most vital elements: the 4Ms. The intention of Age-Friendly Health Systems is to equitably incorporate the 4Ms into existing care, rather than layering them on top, to organize the efficient delivery of effective care.
This integration is achieved primarily through leveraging existing resources within a health system or individual care setting. Many health systems have found they already provide care for many of their older patients that aligns with one or more of the 4Ms. For example, a Community Living Center nursing home in the Veterans Health System in Gainesville, FL, saved 6 hours per week of meeting time by organizing care via the 4Ms (The Institute for Healthcare Improvement, 2024).
To achieve results, such as those in Gainesville, there are two key drivers of age-friendly care: “Assess” and “Act On.” The “Assess” category means that a health system understands how the 4Ms affect care for every older adult, in every interaction. The “Act On” command means a health system has incorporated the 4Ms into care delivery and is documenting them in the care plan (see Figure 2, below). Both drivers need to be supported by factors such as communication and documentation (through the electronic medical record and other methods) across clinical care settings and the continuum of care, including hospitals, ambulatory practices (including primary care practices), convenient care clinics, and nursing homes (including post-acute and long-term care settings, e.g., skilled nursing, rehabilitation facilities, and nursing facilities).
Figure 2
Two Key Drivers of Age-Friendly Health Systems
If health systems can assess and act on the 4Ms for all older adults in their care, recognition by the IHI and the JAHF celebrates their work. Recognition happens at two levels: Level 1: as an Age-Friendly Health System Participant, which means health systems have successfully developed a plan to implement the 4Ms; and Level 2: being Committed to Care Excellence, which means health systems have 3 months of data on older adults who have received the reliable practice of evidence-based interventions using the 4Ms.
While the movement started in the United States, age-friendly care now has global reach. As of August 2024, the Age-Friendly Health Systems movement comprises 5,000 health systems. These health systems are working to reliably deliver evidence-based care in 10 countries: Australia, Brazil, Ireland, Lebanon, Portugal, Qatar, Saudi Arabia, South Korea, the United Arab Emirates, and the United States. In addition, individual champions in more than 53 countries have taken a course on Age-Friendly Health Systems. It is estimated that health systems recognized to date reach more than 3.75 million older adults.
Health Equity
Health equity is foundational to the Age-Friendly Health Systems movement. As stated, the goal of the Age-Friendly Health Systems movement is to provide evidence-based care to all older adults, in an equitable way, across settings of care. In this context, equitable application of age-friendly care “means reliably assessing and acting on the 4Ms regardless of race, ethnicity, language, sexual orientation, gender identity, or social circumstance” (Southey & Henriquez Garcia, 2023).
If a health system can assess and act on the 4Ms for all older adults in their care, they receive formal recognition by the IHI and the JAHF.
Health systems have the flexibility to provide evidence-based care that aligns with the 4Ms, based on What Matters most to the older adult and their care partners. Like the boxes on the “equity” side of the image (below), health systems can select tools that matter to them to assess and act on 4 or more Ms, so that every older adult in every interaction is provided with care as unique as their experiences.
Using an equity lens means understanding and then addressing existing inequities in care for older adults from historically marginalized groups (Southey & Henriquez Garcia, 2023). Older adults from historically marginalized communities suffer from disparate treatment that negatively influences health outcomes, especially if they possess multiple marginalized identities.
A study by The Commonwealth Fund found that “one in four Black and Latinx/Hispanic adults ages 60 and older [in the United States] reported that they have been treated unfairly or have felt that their health concerns were not taken seriously by health professionals because of their racial or ethnic background,” resulting in poor health (The Commonwealth Fund, 2022). Identifying and addressing whether some groups are more or less likely to receive age-friendly care that aligns with the needs and preferences of the older adult and their caregivers is essential for any health system seeking to become Age-Friendly (Southey & Henriquez Garcia, 2023).
Putting the 4Ms into practice means using improvement science and other methods to test small changes to a health system’s workflow (see Figure 4, below). This method reliably integrates equity into the 4M’s implementation from the start, allowing health systems to approach age-friendly care without “adding on” equity. This guidance was shaped by exemplar health systems based on their experience providing equitable age-friendly care, in the Brigham and Women’s Hospital, Houston Methodist Hospital, Oregon Health & Science University, and the University of Chicago’s SHARE Network (Southey & Henriquez Garcia, 2022).
Figure 3
Integrating Equity into Your Age-Friendly Health Systems Journey
Localizing the 4Ms
From global to local, health systems have adapted the 4Ms to meet the needs of the older adults in their community. This includes supplementing the 4Ms framework.
In 2021, Grady Hospital in Atlanta, GA, incorporated Malnutrition into the 4Ms framework when staff noticed that more than 25% of their hospitalized older adults were malnourished. While improvements have been made in recent years, research demonstrates that malnutrition remains a health concern for older adults (Norman et al., 2021). Norman et al. (2021) suggested that malnutrition not only impacts mortality and morbidity but also everyday activity (Mobility), well-being (Mentation), and quality of life (What Matters).
Malnutrition is synergistic to the 4Ms and complementary to age-friendly care. At Grady, to assess and act on malnutrition, nurses screen for malnutrition at intake, looking for signs of weight and muscle mass loss, and diminished hand grip strength, following the ASPEN guidelines. (For more practical tools and tips on how Grady Hospital implements the 5Ms, see The Institute for Healthcare Improvement, 2021.)
Northwell Health and Providence Health, both large-scale systems, have incorporated multi-complexity as their 5Ms—an older adult having multiple, chronic health and mental or behavioral health conditions requiring complex care—into the 4Ms (Kuo & Houtrow, 2016). The flexibility of the 4Ms, and aligning all care through What Matters, allows for this sort of adaptation and localization, depending upon which factors affect the care of older adults in a community, taking a place-based, equity-centered approach to care that’s central the Age-Friendly Health Systems movement.
Age-Friendly Ecosystem
The 4Ms of age-friendly care, while started in the healthcare sector, can be applied across the care continuum and in care for older adults where they live, learn, work, play, or pray. The Age-Friendly Ecosystem is a concept that uses a “collective impact” framework developed by the Collective Impact Forum in 2016 that aligns and structures efforts to achieve greater change, which has proven to be a successful model (Kania & Kramer, 2011). The intention of the ecosystem is to collaborate across the five ecosystem sectors, including cities/communities, public health, employers, universities, and health systems, while centering equity and older adults, as well as their caregivers, in the process.
Many health systems see the value of partnering across sectors, as an extension of providing evidence-based care to all older adults in their communities.
Each sector uses a framework to support and improve the health and care of older adults broadly, such as the 4Ms framework. Within the Age-Friendly Health Systems movement, there is a suite of tools and resources that health systems and other sectors can use to improve care. One of those tools is The Three Keys to Cross-Sector Age-Friendly Care, which are What Matters, Supportive System Structures, and Financial Structures & Policy Landscape. The keys function at different levels of the system, and take a socioecological approach used in public health (Nelson & Saret, 2023).
The framework includes a set of ideas for change that health systems, public health organizations, and community-based partners can adopt that are proven to produce improvement. Some proposed change ideas may apply to individual organizations in public health or healthcare in their role as part of the age-friendly ecosystem, while others require partnering in, across, or outside these sectors (Nelson & Saret, 2023). This is one small way health systems can see themselves as part of the solution.
Figure 4
The Three Keys to Cross-Sector Age-Friendly Care
While cross-sector collaboration is not part of the process to be recognized as an Age-Friendly Health System, many health systems see the value of working with partners across sectors, and view it as an extension of their work to provide evidence-based care to all older adults in their communities. The What Matters element of the 4Ms framework often resonates and is the linchpin connecting age-friendly approaches across sectors and brings a unique opportunity to the work across the ecosystem. In the context of Age-Friendly Health Systems, What Matters is defined as understanding and “aligning care with each older adult’s specific health outcomes, goals, and care preferences, including, but not limited to, end-of-life care, and across settings of care” (Institute for Healthcare Improvement, 2023).
Assessing and acting on What Matters allows health systems and their partners across sectors to use a person-centered approach, which is unique to each adult’s needs and wishes, living out the principle of health equity. Often questions about what matters to older adults will uncover social determinants of health, activities (such as walking their dog) they wish to return to in their community with friends or family, and how they want to contribute to their communities through volunteerism or part-time responsibilities. This is a clear opportunity for sectors in the ecosystem to partner with older adults and their caregivers, to streamline access to services, resources, and returning to their homes.
Below are two examples of how health systems work outside their organization with partners across sectors in their community.
Jefferson Center for Healthy Aging
The Jefferson Center for Healthy Aging is an ambulatory facility and part of the Jefferson Health system in Philadelphia, PA. Part of its approach included work in its system and outside the healthcare sector. In a case study (Jefferson Health, n.d.), the Jefferson Center for Healthy Aging team described how they introduced the 4Ms framework to architecture and design experts from partnerships to inform aging-in-place and smart cities design in their community. The Jefferson Center also described how it is integrating the 4Ms into the curriculum at the Sidney Kimmel Medical College and in its Interprofessional Education programs. Working with businesses and universities on a collective-impact approach will positively affect older adults and future generations to come.
AdventHealth Hendersonville
AdventHealth Hendersonville is a 100-bed hospital with 1,200 employees in Hendersonville, NC (American Hospital Association, 2022). It works in and outside the healthcare sector and has integrated the 4Ms of age-friendly care into its annual strategic and financial planning as well as incorporating age-friendly care into its annual wellness visits for older adult patients. Starting in 2018, AdventHealth Hendersonville’s leadership and lead geriatrician formed a task force comprising healthcare and community partners. Since then, the task force has created a vision board for the care they hope to provide across the care continuum and are working to improve access to healthy food for patients who attend annual wellness visits at AdventHealth Hendersonville.
While these case examples are successful, collaboration across sectors is a challenge. Health systems are a foundational asset to a community, often providing acute health services, employing members of the community, and a source of economic benefit. While these are valuable to communities, healthcare collaboration with other sectors to use these benefits has remained a challenge for health systems and evidence is lacking that this will change (Alderwick et al., 2021).
Conclusion
Health systems have an opportunity to better collaborate with sectors across the Age-Friendly ecosystem. Older adults are living longer and that’s something to be celebrated. With a growing, more diverse population, age-friendly care is needed now more than ever for the future of older adults and their caregivers. Resources from the Age-Friendly Health Systems movement, such as The Three Keys, can be a way for health systems to get started.
Through the lens of the 4Ms, person-centered care delivered in an equitable, reliable way, and aligned with What Matters, needs to be adopted as the standard of care for every older adult. To do this, the Age-Friendly Health Systems movement is part of the solution that provides practical applications to complex problems. Together, we can build a better system so that all older adults can thrive.
Laura Howell Nelson is project director for Age-Friendly Health Systems at the Institute for Healthcare Improvement.
Photo credit/Shutterstock/PattyPhoto
References
Alderwick, H., Hutchings, A., Briggs, A., & Mays, M. (2021). The impacts of collaboration be-tween local health care and non-health care organizations and factors shaping how they work: A systematic review of reviews. BMC Public Health, 21, 753. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-10630-1
American Hospital Association. (2022). Age-friendly health systems case study: AdventHealth Hendersonville. https://www.aha.org/system/files/media/file/2022/02/afhs-cs-advent-hendersonville.pdf
The Commonwealth Fund. (2022). How discrimination in health care affects older Americans, and what health systems and providers can do. https://www.commonwealthfund.org/publications/issue-briefs/2022/apr/how-discrimination-in-health-care-affects-older-americans
The Institute for Healthcare Improvement. (2021). Providing age-friendly care to address health equity. IHI Blog. https://www.ihi.org/insights/providing-age-friendly-care-address-health-equity
The Institute for Healthcare Improvement. (2024, March 1). Centering what matters: The core of age-friendly care. IHI Blog. https://www.ihi.org/insights/centering-what-matters-core-age-friendly-care
The Institute for Healthcare Improvement. (2023). Age-friendly health systems: How to have con-versations with older adults about what matters. https://www.ihi.org/sites/default/files/2023-10/AgeFriendlyHealthSystems_How-to-Have-Conversations-with-Older-Adults-About-What-Matters.pdf
Jefferson Health. (n.d.). Age-friendly case study: Jefferson. https://241684.fs1.hubspotusercontent-na1.net/hubfs/241684/Age-Friendly/Age-Friendly%20Case%20Studies/Age-Friendly_Case_Study_Jefferson_FINAL-02.pdf
Kania, J., & Kramer, M. (2011). Does collective impact really make an impact? Stanford Social Innovation Review. https://ssir.org/articles/entry/does_collective_impact_really_make_an_impact#
Kuo, D. Z., & Houtrow, A. J. (2016). Recognition and management of medical complexity. Pediatrics, 138(6). https://doi.org/10.1542/peds.2016-3021
Nelson, L. H., & Saret, C. (2023). Improving public health and health care for older adults: The three keys to cross-sector age-friendly care. Institute for Healthcare Improvement. www.ihi.org/agefriendly
Norman, K., Haß, U., & Pirlich, M. (2021). Malnutrition in older adults—recent advances and remaining challenges. Nutrients, 13(8), 2764. https://doi.org/10.3390/nu13082764
Southey, C., & Henriquez Garcia, L. (2022). Ensuring equitable age-friendly care. Healthcare Executive. 38(6), 44-45.
Southey, C., & Henriquez Garcia, L. (2023). Focusing on equity at every step of your age-friendly health systems journey. https://241684.fs1.hubspotusercontent-na1.net/hubfs/241684/Age-Friend-ly/Guides%20and%20Toolkits/Focusing%20on%20Equity%20at%20Every%20Step%20of%20Your%20Age-Friendly%20Health%20Systems%20Journey.pdf
Tinetti, M. (2019, January 23). How focusing on what matters simplifies complex care for old-er adults. IHI Blog. https://www.ihi.org/insights/how-focusing-what-matters-simplifies-complex-care-older-adults













