HealthHIV’s Pozitively Aging program works to improve access to services and care coordination for People with HIV (PWH) who are older than age 50, and to improve their health outcomes and quality of life. Through enhancing care coordination, access, engagement, patient-provider communications and health literacy, Pozitively Aging offers medical and health services research education and materials to strengthen that relationship. In addition, it also offers information on self-management of care and health literacy for all older persons with HIV (OPWH).
HealthHIV’s National Resource Center for Care Coordination and Pozitively Aging with HIV
The National Resource Center for Care Coordination and Pozitively Aging with HIV conducts unique, original research and evaluation to advance care coordination for people living and aging with HIV. The National Resource Center is aligned with HealthHIV’s advocacy, medical education, capacity-building and technical assistance, and works to build the capacity of HIV and primary care providers for PWH across a lifespan.
HealthHIV’s State of Aging with HIV Third Annual National Survey
This Survey underscores the ongoing needs and experiences of people aging with HIV, many of whom are among the first generation of people to be diagnosed with HIV.
HealthHIV’s State of Aging with HIV Third Annual National Survey was developed to gather information on the current experiences of OPWH in the United States. It is the only national landscape survey of OPWH. The survey was conducted from October 2022 to January 2023, and included 151 dynamic, adaptive questions asked of individuals older than age 50 or those who had been living with HIV for 15 or more years. It drew from a diverse pool of 673 participants.
Survey questions were reviewed for relevance and comprehensiveness by an advisory board, and the survey was conducted online. It applied a range of statistical techniques, along with thematic analysis of qualitative data (and quotes) to comprehensively explore and capture the full spectrum of participant experiences.
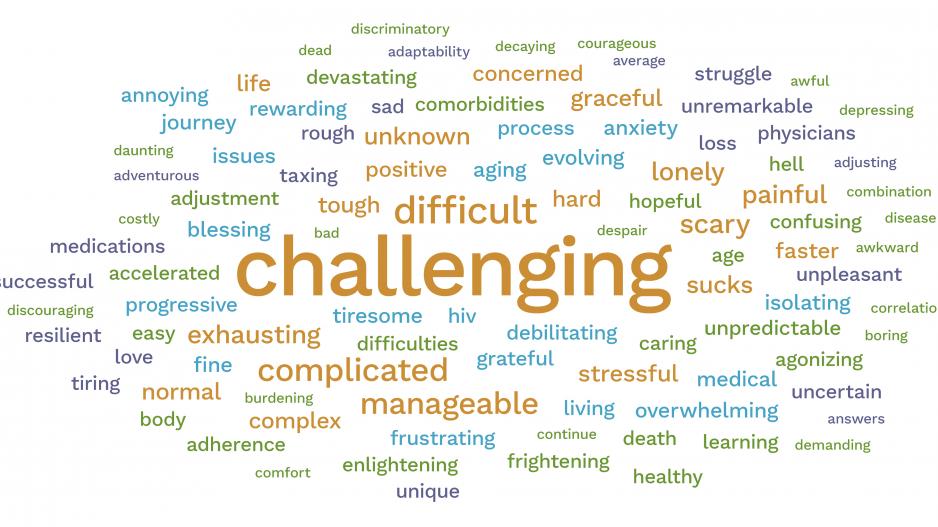
In One Word
Respondents conveyed their fear of the unknown, being unaware of what to expect, and how to anticipate and manage impending challenges. One respondent said they wanted: “More discussion of known or potential HIV related health issues [that] are possible in my future.”
Another respondent proffered a similar sentiment: “Knowledge of what’s [to] come as we age. I am aware that we are living longer, but there is much we don’t know.”
When asked to describe their quality of life in one word, respondents offered a wide range of responses—from “blessed” and “fair” to “lonely” and “poor,” revealing a heterogeneous landscape of experiences. One respondent said: “Quality of life is more valuable to me than [the] mere quantity of it.”
Improving Care Coordination
The demographic shift toward a population that is aging with HIV introduces complex challenges for healthcare systems. Developing effective care models and interventions for OPWH requires a cross-discipline (multidisciplinary team) awareness and understanding of their unique needs.
Critically, the survey revealed that 93% of respondents were older than age 50, with a significant burden of multimorbidity and polypharmacy, making seamless care coordination across specialties imperative. Integrating electronic health records and telehealth, along with fostering cross-sector partnerships, is vital for creating a cohesive healthcare experience for OPWH.
Optimizing Medication Management
With three-quarters of respondents juggling multiple medications daily, strategies to minimize polypharmacy risks are crucial. Comprehensive medication reviews, personalized pharmacotherapy plans and patient education on adherence and polypharmacy can enhance medication management and overall health outcomes.
Addressing Physical and Mental Health Challenges
Given that 64% of respondents report mental health concerns, it is essential to integrate mental health services, physical health screenings and holistic wellness programs into care models. Such an integrated approach ensures that physical and mental health needs are addressed, improving quality of life for OPWH.
‘Addressing the stigma OPWH face requires education, advocacy and policy reform.’
Integrating Geriatric and HIV Care
The survey’s data on mental health concerns and the prevalence of comorbidities emphasize the need for healthcare providers skilled in both geriatric and HIV care. Education and policy changes aimed at enhancing provider competencies in managing the health complexities of OPWH were found to be critical.
Tackling Social Determinants of Health
Survey data also stresses how social determinants like personal agency, social isolation, financial concerns and housing (and worry about long-term care services) impact OPWH’s health and well-being. Collaborative models that connect healthcare services with social support systems can address these challenges, improving OPWH’s overall well-being.
Enhancing Patient Engagement
Survey findings on OPWH and their care engagement stress the need for knowledgeable HIV gerontologists and better care coordination. Engaging OPWH in their care through specialized training for healthcare providers and integrated healthcare approaches is critical.
Combating Stigma
Addressing the stigma OPWH face requires education, advocacy and policy reform. Creating inclusive environments and fostering societal awareness can help mitigate stigma and discrimination, enhancing access to care.
Improving Access to Services
Targeted outreach and education efforts are essential to raise awareness and increase service uptake among older adults, who are underrepresented in HIV services. Tailoring these initiatives to the specific needs and preferences of older populations can improve access to HIV testing, prevention and care.
Creating Age-Friendly Healthcare Environments
Modifying physical spaces, training staff, and delivering services to accommodate the needs of OPWH can create more welcoming healthcare environments. These modifications should focus on accessibility, comfort and respect for OPWH’s unique needs.
Addressing Comorbidities and Mental Health
Integrating preventive care measures, routine screenings and tailored management of comorbidities, along with addressing social determinants of health, is imperative for improving health outcomes among OPWH.
Culturally Competent Care
Ensuring cultural competence and inclusivity in care models for OPWH from diverse backgrounds means being aware that healthcare staffing is diverse and comprehensively trained in cultural competency. Also crucial are inclusive policies that respect the diversity of the aging HIV population.
Conclusion
Optimizing care models and interventions that effectively address the needs of OPWH requires a collaborative, strategic and compassionate approach. By focusing on the outlined points, patients, healthcare providers, navigators, researchers, policymakers and payers can work together to create a healthcare landscape that is inclusive, equitable and responsive to the needs of older adults living—and aging—with HIV across a lifespan.
The call for building a competent workforce of HIV gerontologists, improving care coordination, addressing social determinants of health, ensuring access to stable housing, and urging policymakers to consider the broad range of factors affecting OPWH underscores the urgency to improving clinical care, together with quality of life.
Our work highlights the struggles of OPWH against a backdrop of polypharmacy, multimorbidity, mental illness and escalating care barriers, painting a portrait of frustration and ire. Faced with compounding challenges and varying health outcomes, and toll from a lifelong (15+ years’) effort of HIV management, today’s picture of aging with HIV for those ages 50 and older has meant resilience in the face of long-term care needs.
Yet, with additional burdens of ageism and other minority stressors, a glimmer of positivity shines through from 28% of survey respondents, who describe their journey with words like “manageable” and “hopeful”—providing a stark contrast to the 72% who depict their quality of life with less joy. In short, our work shows that for OPWH, there is (and was) truly “Nothing about us without us.”
Scott D. Bertani, MNM, PgMP, is director of Advocacy at HealthHIV in Washington, DC.
Photo credit: theshots.co













