Abstract
The intersection of climate change and population aging presents challenges for an increasingly older U.S. labor force. Exposure to extreme heat at work is associated with mortality and morbidity, but little is known about how exposure to heat at work relates to work disability, especially among vulnerable subgroups. In this preliminary analysis of work disability and occupational heat exposure, we find that men, Black, and Latino workers ages 50 and older are more likely to work in heat-exposed occupations and to report work disability. We offer policy suggestions for mitigating the impact of extreme heat on U.S. workers.
Key Words
climate change, adaptation planning, heat, occupational risk, health disparities, work disability
In the coming decades, the effects of climate change, including the frequency and severity of heat waves, will increase to the point of becoming a “new normal” (e.g., Su et al., 2023). This future will unfold along with population aging and an older workforce (e.g., Carr et al., 2024). Since 2000, the proportion of workers ages 60 and older in the U.S. labor force has doubled (National Academies of Sciences, Engineering, and Medicine, 2022). Exposure to extreme heat is associated with higher mortality rates, adverse health outcomes, job injuries, and reduced work productivity, especially among older and marginalized groups (Berberian et al., 2022). Yet little is known about how occupational heat exposure relates to work disability.
Disparities in Risk of Exposure to Heat Sensitive Occupations
The effects of extreme heat may disproportionately impact certain classes of workers, specifically those who work outdoors or in indoor settings with inadequate climate control. There is some evidence that racial and ethnic minorities may be overrepresented in vulnerable jobs (e.g., Tipaldo et al., 2024), which are often low-income and accept low educational attainment. The effect of occupational heat exposure also may be exacerbated in low socioeconomic status (SES) communities because of pre-existing conditions, such as higher rates of diabetes.
The Role of Policy in Mitigating the Health and Workforce Impact of Extreme Heat
In 2024, the Biden administration attempted to provide additional protections against heat exposure and its effects on the job (Davenport & Weiland, 2024), but the future of those regulations remains uncertain. At a more local level, several states and municipalities have begun mandating protections, such as requiring water and more rest breaks during heat waves and having a plan for workers who develop heat-related illness while working (Lander, 2024). However, these measures have not yet been enacted nationwide and often do not apply to informal workers, such as subcontractors, delivery workers, and street vendors.
Contribution
This article addresses an increasingly relevant topic as climate change and demographic aging intersect. We first review existing empirical and theoretical understandings of the role of extreme heat in work disability (Section I) and pay close attention to the life-course factors that place certain populations at greater risk for work disability due to heat exposure (Section II). Next, we conduct a preliminary analysis of work disability and occupational heat exposure using a nationally representative dataset of U.S. adults older than age 50 (Section III). We conclude by highlighting public health measures and policy tools for mitigating occupational heat exposure on work disability (Section IV) and presenting the current state of data on this topic and how we conducted our analysis (Section V). This article provides a launching point for future research on the health implications of occupational heat exposure across the life course.
I. Extreme Heat: Implications for Work Disability
Exposure to extreme heat is one of the most significant public health concerns to prepare for in the coming decades. Heat waves are some of the deadliest disasters (Ebi et al., 2021). The risk of occupational heat strain is more prevalent in certain occupations and industries (e.g., agriculture, construction), and research tends to focus on those occupations or on specific heat waves (Ioannou et al., 2022). Research has shown that occupational exposure to heat is correlated with elevated risk for heat-related mortality and morbidity (see recent reviews, e.g., Flouris et al., 2018). This research primarily focuses on immediate outcomes, such as emergency room visits for heat stroke in industrial settings (Spector et al., 2019). Much less is known about the link between occupational heat exposure over the life course (Mazzei, 2024) and its association with work disability.
‘Racial minorities, immigrants, men, and individuals with low SES may be more vulnerable to the effects of extreme heat.’
The health effects of extreme heat may be seen immediately and long term. High heat can worsen pre-existing chronic health conditions, such as diabetes, respiratory diseases, and cognitive or psychiatric conditions (New York City Department of Health and Mental Hygiene, 2024). During and immediately after heat exposure, workers may experience dehydration, heat stroke, heat cramps, and exhaustion (Chaseling et al., 2021). Hot days also may be associated with a greater risk of workplace accidents and injury (Spector et al., 2019). Over the long term, a small but growing body of evidence has found severe heat stress can effect changes in DNA that result in accelerated aging (Choi & Ailshire, 2025).
Disability is often examined in frameworks beyond the medical model. These alternative models view disability as a result of interactions between individuals and their environment. These range from simple to more complex models that connect health conditions, impairments or functional limitations, and social and contextual factors, including policies. While the natural environment, such as climate and weather, influences work, health, and work disability, the natural environment is often implied rather than explicitly addressed in traditional theoretical frameworks of work disability.
II. Those Most at Risk
The life-course pathways that link extreme heat exposure to poor health and ultimately work disability are complex and multifaceted. Figure 1, below, depicts the factors we hypothesize will strengthen or weaken the relationship between extreme temperature, poor health, and ultimately work disability. In this model, the relationship between heat-exposed occupation and poor health is magnified in vulnerable populations. It may be weakened or disappear in others, depending on factors such as working conditions and sociodemographics. Specifically, we hypothesize that those who work in occupations with greater outdoor exposure (e.g., agriculture, construction; see Gubernot et al., 2014) and in a subset of indoor jobs without climate control bear a disproportionate impact from extreme heat. The most recent (2023) Bureau of Labor Statistics Occupational Requirement Survey revealed that 33% of civilian workers are engaged in occupations requiring outdoor exposure (Bureau of Labor Statistics, 2024). Recent journalism also has highlighted indoor occupations lacking sufficient climate control, like warehouse, restaurant kitchen, and night-shift custodial work, or aircraft cabin cleaners (e.g., Davenport & Weiland, 2024; Mazzei, 2024).
Figure 1. Conceptual Model of the Relationship Between Exposure to Extreme Temperatures and Work-Related Disability
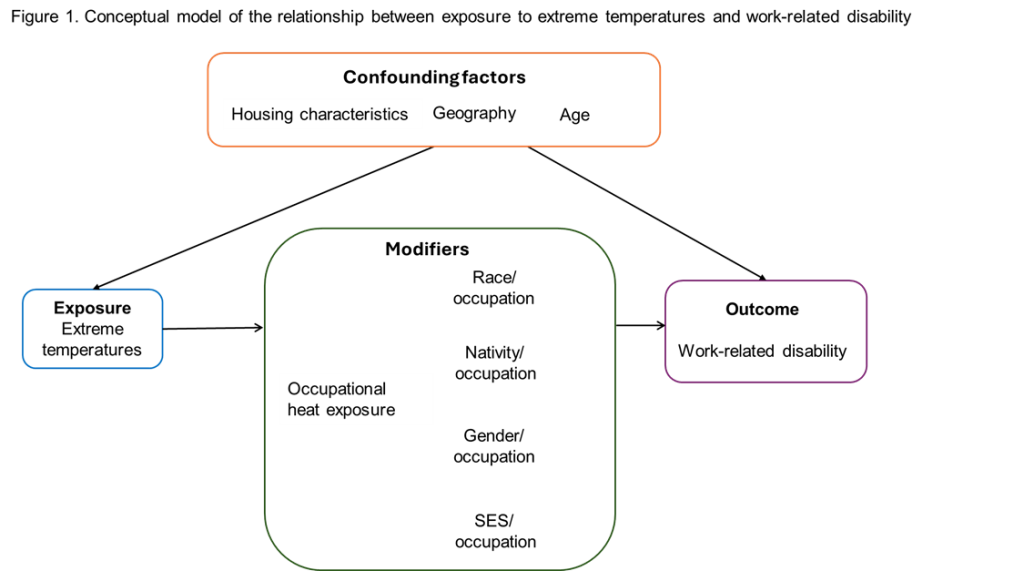
Additionally, racial minorities, immigrants, men, and individuals with low SES may be more vulnerable to the effects of extreme heat, which may lead to poor health and ultimately work disability (compared to white individuals, the native born, women, and those of higher income). First, certain groups (by gender, race/ethnicity, nativity, and SES) are often overrepresented in specific jobs and therefore, may have more exposure to heat-sensitive work. Often lower paid, outdoor jobs and indoor jobs with high heat exposure are filled by marginalized workers (Acharya et al., 2018), such as Latinos and immigrants. These occupations also have a higher proportion of male workers (Bureau of Labor Statistics, 2021).
Second, those of low SES and racial minorities are more likely to have comorbidities (e.g., diabetes or being overweight), which can compound risks from heat exposure. Third, jobs occupied by marginalized workers may adhere less often to safety regulations (Leeth & Ruser, 2006) and be less likely to offer employer-sponsored benefits (e.g., health insurance; Claxton et al., 2024) that mitigate the health impact of extreme heat.
For example, imagine two workers (Alex and Jamie) who spend most of their working lives in the same southwestern city and are exposed to the same number of high-heat days, but differ in meaningful ways. Alex is a college-educated professional who works in an air-conditioned office, commuting via a private vehicle from a home with central air conditioning. Alex’s job provides extensive benefits, including private health insurance, so Alex has a regular source of preventive healthcare and covered visits if sick or injured.
Jamie works in construction and is mostly outside, even during heat waves. Due to lower pay, Jamie sometimes relies on public transportation, which adds commute time and increases exposure to high heat when waiting for the bus. Jamie relies on a window air-conditioning unit at home, which is sometimes unaffordable. Jamie’s job is seasonal and temporary, so Jamie’s employer is not mandated to provide benefits, including health insurance. Therefore, Jamie has no regular source of preventive care and often delays doctor’s visits even when feeling sick or for minor injuries.
‘U.S.-born individuals (22%) are more likely than foreign-born individuals (17%) to report that health limits their ability to work.’
Over his working life, Alex has very little on-the-job heat exposure and is therefore unlikely to stop working prematurely due to heat-induced disability. Jamie, in contrast, is exposed for eight or more hours each high-heat workday and is also more likely to be exposed when at home or on the way to or from work. Therefore, Jaime is much more likely to suffer health effects from high heat, which, without workplace protections, accommodations, or access to healthcare, may result in work disability.
III. The Association Between Exposure to Heat-Sensitive Occupations and Work Disability
We conducted an analysis of work disability and heat exposure at work using a nationally representative dataset of U.S. adults older than age 50. Occupations were classified as heat sensitive in four categories (for details on our methodology see Section V): (1) exposed to outdoor conditions, (2) works inside but without climate control, (3) two or more heat sensitive exposures, and (4) unexposed to heat.
First, we compared rates of work disability by category of heat sensitive occupation (HSO; see Figure 2, below). At age 55, we estimate that about a fifth (19%) of individuals who worked in “unexposed” jobs report that health limits their ability to work. In contrast, a quarter or more individuals in all three exposed HSO groups are estimated to report that health limits their ability to work at age 55.
Figure 2. Is There an Association Between Working in Heat-Sensitive Occupations and Health Limiting Work? Predicted Probabilities of Reporting that Health Limits Work by Heat Sensitive Occupation (HSO) Classification of Longest Held Job at Baseline at Age 55
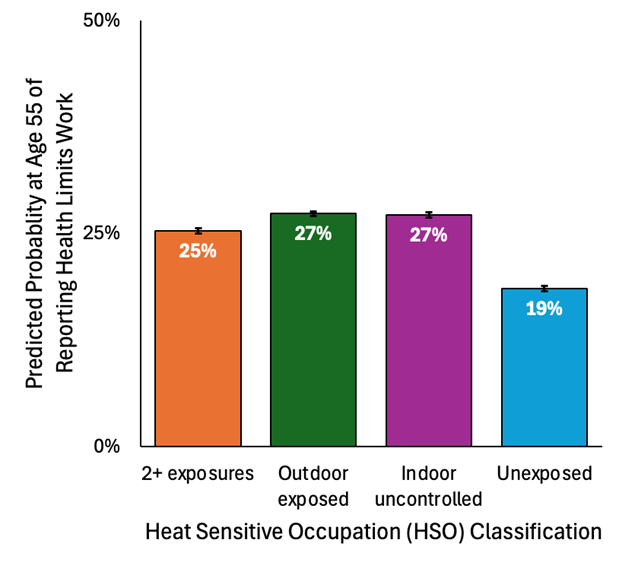
Note: Data: Health and Retirement Study (HRS) 1992–2020; linear probability models estimated with robust standard errors to account for multiple observations per respondent, models control for age, sex, race/ethnicity, nativity and education; post-regression predicted probabilities estimated at age 55 (covariates held at observed values), 95% Confidence Intervals.
Next, we look at the sociodemographic characteristics of each HSO (see Figure 3, below). For comparison, dashed lines show the overall distribution of each subgroup in the sample. Results show stark gender, nativity, race/ethnicity, and educational differences by HSO, providing evidence that specific subgroups may be at increased risk of health impairment due to exposure to extreme heat at work. For example, men are overrepresented in occupations with two or more exposures (87%) and indoor uncontrolled occupations (57%) compared to the percent of men in the sample overall (52%). Foreign-born, Black, and Latino respondents are also overrepresented in heat-exposed occupations compared to their distribution in the overall sample. In terms of educational attainment, in the overall sample, 22% of respondents hold a BA or more, but 32% of those working in non-heat-sensitive occupations have this level of educational attainment compared to 3–5% in the other three HSO categories. Conversely, in the full sample, 20% of respondents have less than a high school degree, but this level of educational attainment is more prevalent in all three HSO categories that are exposed to extreme heat. This indicates considerable vulnerability to exposure to extreme heat for those with lower educational attainment.
Figure 3. Who Is Exposed to Heat Sensitive Occupations (HSO)? Sociodemographic Characteristics by Heat Sensitive Occupation Classification
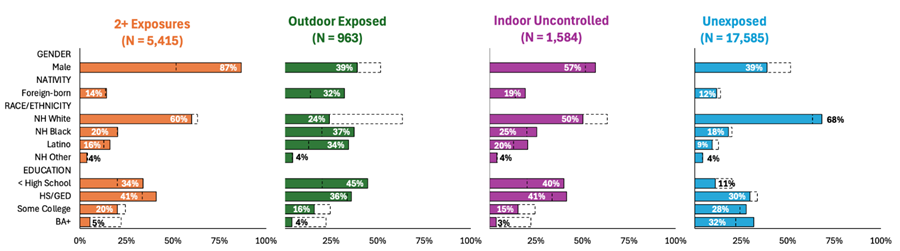
Note: Data: HRS 1992–2020; distribution of sociodemographic characteristics of workers (1 observation per respondent) within each HSO category. Dotted lines indicate the overall distribution for the entire sample for comparison.
Finally, we look at the sociodemographic characteristics of individuals who report that their health limits their ability to work (see Figure 4, below). Here we see that women (22%) are more likely than men (19%) to report that their health limits their work. This difference may be attributable to higher mortality rates among men (selection), whereby women stay in the workforce longer but are more disabled (Owens, 2002; Singh & Siahpush, 2001). We also see that U.S.-born individuals (22%) are more likely than foreign-born individuals (17%) to report that health limits their ability to work. This may be because foreign-born workers may not be able to access work accommodations and may have barriers to exiting the workforce even if they are disabled compared to U.S.-born workers (Gignac et al., 2018; Lopez & Slavov, 2020). In terms of race and ethnicity, we estimate that more than a quarter (27%) of non-Hispanic Black respondents report that health limits their ability to work, and 22% of Latino and other non-white respondents report similarly. This is compared to less than a fifth (19%) of non-Hispanic white respondents at this age. Finally, there is evidence that the likelihood of health limiting work is lower for those with a college degree (BA) than for those without: While 11% of individuals with a BA are estimated to report that health limits work, almost a third of those without a high school degree (29%), more than a fifth of those with a high school degree (22%), and those with some college (21%) are estimated to report that health limits their ability to work.
Figure 4. Who Is Most Likely to Report that Health Conditions Limit their Work? Predicted Probabilities of Health Conditions Limiting Work by Sociodemographic Characteristic at Age 55
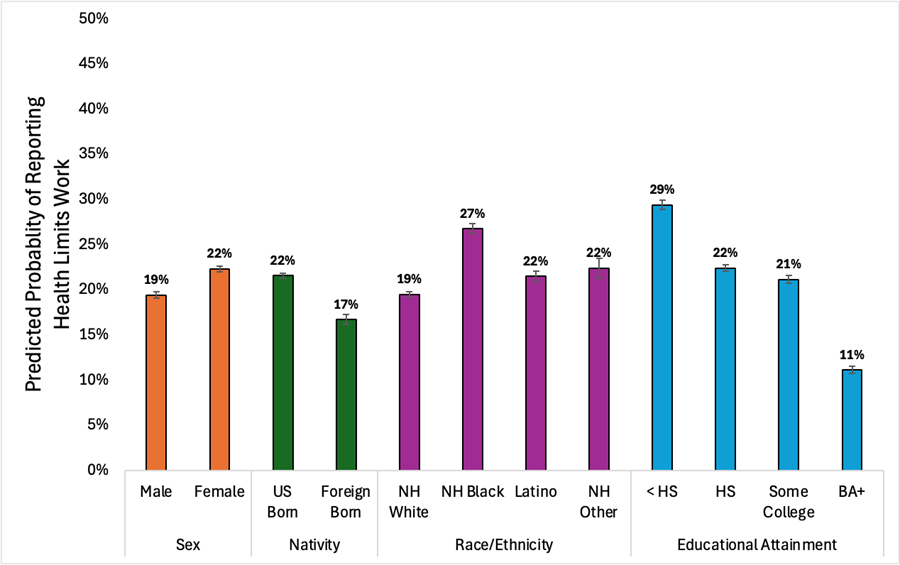
Note: Data: HRS 1992–2020; linear probability models estimated with robust standard errors to account for multiple observations per respondent, models control for age, sex, race/ethnicity, nativity, and education; post-regression predicted probabilities estimated at age 55 (covariates held at observed values), 95% Confidence Intervals.
These results represent a preliminary analysis of the relationship between work in heat-sensitive jobs and work disability. Our findings also highlight subgroups that may be more likely to experience the detrimental impact of extreme heat exposure. This analysis does not identify locations with high rates of extreme heat per year, or the specific subgroups employed in these places. For example, migrant agricultural workers in Texas may have fewer protections and more exposure to extreme heat, magnifying the implications on work disability, than their counterparts in California, due to differences in climate, legislation, adherence to safety regulations, and state-provided health insurance programs for migrants (Bustamante et al., 2023). This is an active and urgent area of research, and future studies should consider specific places that are at risk and measure long-term exposure to extreme heat.
IV. Public Health and Policy Implications
Two broad approaches—primary and tertiary prevention—have been used to address occupational exposures to extreme heat. Primary prevention attempts to prevent extreme heat exposures in the workplace by mandating appropriate occupational safeguards. For example, in 2024, the Occupational Safety and Health Administration (OSHA) proposed a rule requiring employers nationwide to evaluate heat risks and to develop an injury and illness prevention plan to enact preventive measures (such as providing water and rest breaks) during extreme heat. The proposed rule also would require employers to protect indoor workers from excessive heat and develop a plan to protect new or returning workers who may be unaccustomed to high heat (indoors or outdoors). Employers also would be required to have plans to identify and respond to workers showing symptoms of heat-related illness. However, the rule is under review at the Office of the Federal Register (OFR) and has not yet been enacted (OSHA, 2024). It is unclear whether the current administration will continue to support the proposal. This proposed federal response would ensure workers nationwide have equal and comprehensive protection.
Vocational training is needed for workers who can no longer work in heat-exposed occupations but are not at retirement age.
Some states, and, in some cases, cities, also have led the way in addressing heat-related occupational exposures through local regulations. For example, a recent report from the NYC Comptroller (Lander, 2024) recommended policy changes that incorporated those proposed at the state and federal levels, but also included provisions for new workers who may not be acclimatized to working in high-heat conditions, developing city-wide guidelines for workers during high-heat and low-air quality days, and expanding bathroom access, particularly for delivery and other workers without a fixed place of employment. Other examples include:
- Phoenix recently passed an ordinance protecting employees of city contractors from extreme heat while working;
- California’s Heat Illness Prevention Standard covers outdoor workers;
- Washington State’s Outdoor Heat Exposure Rule covers outdoor workers;
- Oregon’s Heat Illness Law covers indoor and outdoor workers;
- Minnesota’s Indoor Ventilation and Temperature in Places of Employment covers indoor and outdoor workers;
- Colorado’s Agricultural Labor Conditions Rules for heat; and
- New York State has pending legislation to address extreme heat.
These regulations vary, but most require employers to provide shade, access to water, and rest breaks during high-heat days. Some also address air quality through measures such as requiring PPE when air quality drops below a certain threshold. However, indoor workers exposed to high heat (such as warehouse and restaurant workers) and contractual or informal workers (such as food delivery workers) often have reduced or no protections.
Tertiary prevention approaches would provide resources to lessen the economic and health burden of those suffering from previous exposures (Prina et al., 2020). Examples of these include:
- Increasing access to disability funding (such as sick leaves, Workers’ Compensation, Supplemental Security Income, Social Security Disability Insurance);
- Expanding healthcare access to workers in occupations impacted by extreme heat, which may not provide employer-sponsored health insurance (especially to marginalized workers who may not be eligible for public health insurance programs); and
- Vocational training for workers who can no longer work in heat-exposed occupations but are not at retirement age.
- Recognition of the disparities in who works in heat-sensitive occupations and their heightened risk of work disability, as we have identified here, serves as an important starting point for developing more effective health policies.
V. Getting Under the Hood—How Our Estimates Were Created
To assess the relationship between exposure to heat-sensitive occupations and work disability, in Section III we analyzed the premier source of data on older adults in the United States, the Health and Retirement Study (HRS). The HRS began in 1992 and is a nationally representative, longitudinal study of Americans older than age 50. HRS asks respondents whether a health impairment or problem limits the type or amount of paid work they can do and collects data on occupations of respondents. To assess the extent to which an individual may have been exposed to extreme heat due to their job, we matched the longest-held job reported by each individual in the HRS at their first interview with occupation-specific job characteristics collected by the U.S. Department of Labor through the Occupational Information Network (O*NET) survey. O*NET includes three job characteristics that indicate potential exposure to extreme heat: 1) outdoors exposed to weather; 2) outdoors under cover; and 3) indoors but not environmentally controlled. We created a summary measure for each HRS respondent indicating the extent to which the job category of their longest-held job was a heat-sensitive occupation (HSO) with the following mutually exclusive categories:
- Top quartile of jobs involving outdoor exposure (no cover),
- Top quartile of jobs involving indoor work without environmental control, jobs involving the top quartile for two or more of these characteristics, and
- Jobs not involving risk for extreme heat exposure (lower 3 quartiles for all three types of exposure).
We then classified the longest-held job reported by each HRS respondent at first interview into one of the HSO categories.
The HRS is a critical window into older Americans’ working, pre-retirement, and retirement lives, but there are some limitations to using these data with environmental exposures over time (e.g., Choi & Ailshire, 2025). O*NET provides an important source of data on occupational characteristics, but the three measures they include that indicate heat sensitivity are not the only measures that could be included. Some pertinent information about transitions from work to disability or retirement may be better studied using complementary mixed-methods research, instead of survey data like HRS. Such research was built into the recent structure of the SSA-funded Retirement and Disability Research Center network, now defunded. Without it, these questions will likely remain unaddressed in the foreseeable future.
How many workers, which ones, and under what conditions they work, will be increasingly important to understand in the decades ahead while more older Americans remain in the workforce and temperatures continue to rise. This will require investments in data as a backbone for efficient and targeted policy to protect the nation’s increasingly older workforce.
Mara Getz Sheftel, PhD, is an instructor in the Department of Health Behavior, Society and Policy, at the Rutgers School of Public Health, in Piscataway, NJ, and the Center for State Health Policy at the Rutgers Institute for Health, Healthcare and Aging, in New Brunswick, NJ. She may be contacted at mara.sheftel@rutgers.edu. Jennifer Brite, DrPH, is an assistant professor in the Department of Nutrition and Public Health at Hunter College in New York City, and at the CUNY Institute for Demographic Research, New York City. Na Yin, PhD, is an associate professor at the Marxe School of Public and International Affairs, in Baruch College, New York City, and at the CUNY Institute for Demographic Research. Deborah Balk, PhD, is a professor at the Marxe School of Public and International Affairs, and the CUNY Institute for Demographic Research.
Photo caption: Gardener of a municipality watering plants and trees in city street during a drought and anomalous heat.
Photo credit: Shutterstock: Tricky_Shark
References
Acharya, P., Boggess, B., & Zhang, K. (2018). Assessing heat stress and health among construction workers in a changing climate: A review. International Journal of Environmental Research and Public Health, 15(2), 247. https://doi.org/10.3390/ijerph15020247
Berberian, A. G., Gonzalez, D. J. X., & Cushing, L. J. (2022). Racial Disparities in climate change-related health effects in the United States. Current Environmental Health Reports, 9(3), 451–464. https://doi.org/10.1007/s40572-022-00360-w
Bureau of Labor Statistics. (2021). Women in the labor force: A databook (1092). United States Department of Labor. https://www.bls.gov/opub/reports/womens-databook/2020/
Bureau of Labor Statistics. (2024, February 8). Occupational requirements in the United States – 2023 [News release]. United States Department of Labor. https://www.bls.gov/news.release/archives/ors_02082024.pdf
Bustamante, A. V., Beltrán, L. F., Cuadros, N. N., Zeng, X. L., & Gonzalez, S. R. (2023). Implementation lessons from the 2022 Medi-Cal expansion to undocumented adults aged fifty and above. Latino Policy & Politics Institute. https://latino.ucla.edu/research/lessons-2022-adult-medical-expansion/
Carr, D., Falchetta, G., & Sue Wing, I. (2024). Population aging and heat exposure in the 21st century: Which US regions are at greatest risk and why? The Gerontologist, 64(3), gnad050. https://doi.org/10.1093/geront/gnad050
Chaseling, G. K., Iglesies-Grau, J., Juneau, M., Nigam, A., Kaiser, D., & Gagnon, D. (2021). Extreme heat and cardiovascular health: What a cardiovascular health professional should know. Canadian Journal of Cardiology, 37(11), 1828–1836. https://doi.org/10.1016/j.cjca.2021.08.008
Choi, E. Y., & Ailshire, J. A. (2025). Ambient outdoor heat and accelerated epigenetic aging among older adults in the US. Science Advances, 11(9), eadr0616. https://doi.org/10.1126/sciadv.adr0616
Claxton, G., Rae, M., Winger, A., Wager, E., & Byers, E. (2024). Employer health benefits: Annual survey. KFF. https://files.kff.org/attachment/Employer-Health-Benefits-Survey-2024-Annual-Survey.pdf
Davenport, C., & Weiland, N. (2024, May 25). ‘New territory’ for Americans: Deadly heat in the workplace. The New York Times. https://www.nytimes.com/2024/05/25/climate/extreme-heat-biden-workplace.html
Ebi, K. L., Capon, A., Berry, P., Broderick, C., Dear, R. de, Havenith, G., Honda, Y., Kovats, R. S., Ma, W., Malik, A., Morris, N. B., Nybo, L., Seneviratne, S. I., Vanos, J., & Jay, O. (2021). Hot weather and heat extremes: Health risks. The Lancet, 398(10301), 698–708. https://doi.org/10.1016/S0140-6736(21)01208-3
Flouris, A. D., Dinas, P. C., Ioannou, L. G., Nybo, L., Havenith, G., Kenny, G. P., & Kjellstrom, T. (2018). Workers’ health and productivity under occupational heat strain: A systematic review and meta-analysis. The Lancet Planetary Health, 2(12), e521–e531. https://doi.org/10.1016/S2542-5196(18)30237-7
Gignac, M. A., Ibrahim, S., Smith, P. M., Kristman, V., Beaton, D. E., & Mustard, C. A. (2018). The role of sex, gender, health factors, and job context in workplace accommodation use among men and women with arthritis. Annals of Work Exposures and Health, 62(4), 490–504. https://doi.org/10.1093/annweh/wxx115
Gubernot, D. M., Anderson, G. B., & Hunting, K. L. (2014). The epidemiology of occupational heat exposure in the United States: A review of the literature and assessment of research needs in a changing climate. International Journal of Biometeorology, 58(8), 1779–1788. https://doi.org/10.1007/s00484-013-0752-x
Ioannou, L. G., Foster, J., Morris, N. B., Piil, J. F., Havenith, G., Mekjavic, I. B., Kenny, G. P., Nybo, L., & Flouris, A. D. (2022). Occupational heat strain in outdoor workers: A comprehensive review and meta-analysis. Temperature, 9(1), 67–102. https://doi.org/10.1080/23328940.2022.2030634
Lander, B. (2024). Safeguarding Outdoor Workers in a Changing Climate. Bureau of Labor Law and Bureau of Policy and Organizing. https://comptroller.nyc.gov/wp-content/uploads/documents/Safeguarding-Outdoor-Workers-in-a-Changing-Climate.pdf
Leeth, J. D., & Ruser, J. (2006). Safety segregation: The importance of gender, race, and ethnicity on workplace risk. The Journal of Economic Inequality, 4(2), 123–152. https://doi.org/10.1007/s10888-005-9008-2
Lopez, M. J., & Slavov, S. (2020). Do immigrants delay retirement and social security claiming? Applied Economics, 52(10), 1105–1123. https://doi.org/10.1080/00036846.2019.1659492
Mazzei, P. (2024, October 26). This Florida farmworker is 75 and still toiling in the heat. The New York Times. https://www.nytimes.com/2024/10/26/us/florida-farmworkers-heat.html
National Academies of Sciences, Engineering, and Medicine. (2022). The emerging older workforce. In Understanding the aging workforce: Defining a research agenda. National Academies Press. https://doi.org/10.17226/26173
New York City Department of Health and Mental Hygiene. (2024). 2024 NYC heat-related mortality report. https://a816-dohbesp.nyc.gov/IndicatorPublic/data-features/heat-report/
Occupational Safety and Health Administration. (2024). Heat injury and illness prevention in outdoor and indoor work settings rulemaking. United States Department of Labor. https://www.osha.gov/heat-exposure/rulemaking
Owens, I. P. F. (2002). Sex differences in mortality rate. Science, 297(5589), 2008–2009. https://doi.org/10.1126/science.1076813
Prina, A. M., Wu, Y.-T., Kralj, C., Acosta, D., Acosta, I., Guerra, M., Huang, Y., Jotheeswaran, A. T., Jimenez-Velazquez, I. Z., & Liu, Z. (2020). Dependence-and disability-free life expectancy across eight low-and middle-income countries: A 10/66 study. Journal of Aging and Health, 32(5–6), 401–409. https://doi.org/10.1177/0898264319825767
Singh, G. K., & Siahpush, M. (2001). All-cause and cause-specific mortality of immigrants and native born in the United States. American Journal of Public Health, 91(3), 392. https://doi.org/10.2105/ajph.91.3.392
Spector, J. T., Masuda, Y. J., Wolff, N. H., Calkins, M., & Seixas, N. (2019). Heat exposure and occupational injuries: Review of the literature and implications. Current Environmental Health Reports, 6(4), 286–296. https://doi.org/10.1007/s40572-019-00250-8
Su, W., Marvel, K., Delgado, R., Aarons, S., Chatterjee, A., Garcia, M. E., Hausfather, Z., Hayhoe, K., Hence, D. A., Jewett, E. B., Robel, A., Singh, D., Tripati, A., & Vose, R. S. (2023). Climate trends. In Fifth national climate assessment. U.S. Global Change Research Program.
Tipaldo, J. F., Balk, D., & Hunter, L. M. (2024). A framework for ageing and health vulnerabilities in a changing climate. Nature Climate Change, 14, 1125–1135. https://doi.org/10.1038/s41558-024-02156-2













