Abstract
This article connects adverse childhood experiences (ACEs), resultant health and chronic conditions, and social isolation. Black Americans are at higher risk of chronic conditions and likely to report more ACEs. Black American caregivers and care receivers are in poorer physical and cognitive health in later life and at higher risk for social isolation. But strong kinship ties, lower caregiver burden, resiliency, and religiosity may prove protective against socially isolation. Recommendations include implementing strength-based interventions, further research, and policy requiring providers to use ACEs in screening for social isolation risk.
Key Words:
social isolation, ACEs, kinship ties, caregiver burden, resiliency, religiosity
Nearly 44 million adults in the United States serve as unpaid caregivers, providing care for an average of twenty-four hours per week and up to as many as forty-one hours per week (AARP and National Alliance for Caregiving, 2020). Caregivers are at risk of experiencing social isolation and becoming disconnected from social networks and community resources, due to overwhelming caregiving tasks, the lack of availability and access to resources in the community and deteriorating physical and mental health.
Social isolation and its health and social impacts on the older population have increasingly become a focal public health issue in policy and research. A relatively recent and attention-grabbing headline noted, “Loneliness Is as Lethal as Smoking 15 Cigarettes Per Day” (Morin, 2018), which has also been emphasized by AARP and used in countless news articles. In the United States, approximately 24 percent of adults ages 65 and older are isolated, and that number is rising (Cudjoe et al., 2018; Frank, 2018).
As life expectancy has increased over the past several decades, so has the risk of developing chronic diseases leading to frailty, disability, and the need for complex care. This increase also is associated with a need for more care, which is most often provided by a family caregiver. The emotional and physical demands required of caregivers place them at greater risk for social isolation and feelings of loneliness (AARP and National Alliance for Caregiving, 2020).
When looking for solutions to tackle social isolation, there must be an understanding of how multiple factors contribute to this circumstance among family caregivers. Moreover, might personal and cultural experiences be considered as solutions? Though there is acknowledgment that early life experiences influence the life course and aging experience, this sentiment has not crossed over to studies of social isolation. It is known that physical and cognitive health decline can serve as risk factors, but the idea that social isolation risk factors can begin in early life should also be considered. In particular, adverse childhood experiences (ACE) should be included as risk factors for social isolation among family caregivers and-or older adult care receivers.
Adverse Childhood Experiences
ACEs are traumatic events experienced before age 18. Kaiser Permanente, in partnership with the Centers for Disease Control and Prevention (CDC), conducted the original, cross-sectional ACE study from 1995 to 1997. It involved two waves of surveying more than 17,000 members of the Kaiser Health Plan in San Diego, California. The entire sample was mostly white, older (age 50 and older), and had a college degree. The study investigated the impact of childhood trauma on health and well-being in adulthood (Felitti, et al., 1998). The study’s ten-item questionnaire asked about events of physical, sexual, and psychological abuse, neglect, and other instances of household dysfunction, including witnessing intimate partner violence, substance abuse, parental divorce or separation, mental illness and imprisonment (of a household member). From these categories, an ACE score was developed, measuring the number of traumatic events, from one to ten, that respondents experienced before age 18 (Felitti, et al., 1998).
The emotional and physical demands required of caregivers place them at greater risk for social isolation and feelings of loneliness.
The research findings suggested that 52 percent of participants experienced at least one ACE, and 6.2 percent experienced four or more ACEs. Substance abuse in the household was the most prevalent ACE; more than 25 percent of respondents reported living with someone who was an alcoholic or with someone who used street drugs (Felitti et al., 1998). In 2009, the CDC added an ACE module to the Behavioral Risk Factor Surveillance System (BRFSS) and has continued to collect ACE data from U.S. states. From the 2011 to 2014 BRFSS data, more than 23 percent of study participants have reported one ACE, and more than 15 percent have reported four or more ACEs. Emotional-psychological abuse was the most reported ACE, at 34 percent. Of those who reported experiencing ACEs, more than 60 percent reported experiencing one or more ACEs (Merrick et al., 2018).
ACEs, Health, and Alzheimer’s Disease
ACEs seem to be a focal point mostly for people in social work and other fields who study and interact with parents and children. However, ACEs have begun to catch the attention of those studying aging issues. ACEs have been found to have a long-term impact on health behaviors and health conditions in late life. Some studies have found that high ACE scores are associated with lower health-related quality of life (Corso et al., 2008) and higher mortality and morbidity in adulthood (Gilbert, et al., 2015). Not surprisingly, ACEs are related to poor health, and can contribute to the development of chronic illnesses such as heart disease, chronic obstructive pulmonary disease, and cancer in later life (Dong et al., 2004; Anda et al., 2008; Brown, Thacker and Cohen, 2013). Taken together, over a life course people with higher ACE scores will enter older adulthood in poorer health compared to those who have fewer childhood adversities. A salient finding on ACEs’ impact in late life is their association with cognitive impairment, such as Alzheimer’s disease. In a report from the Center of Youth Wellness (2014), those who reported four or more ACEs were eleven times more likely to develop Alzheimer’s disease than those who reported no ACEs.
Another study on Japanese older adults found that those who reported three ACEs had a greater risk of developing dementia compared to those with no ACEs (Tani, Fujiwara, and Kondo, 2020). Because of the health impact of ACEs, those who report high ACEs likely will have complex care needs in later life. This could negatively impact both the caregivers’ and older adult care receivers’ social networks. Research suggests that caregivers to people with complex care are at greater risk for isolation. Therefore, it is possible that Black American caregivers and-or care receivers might be at greater risk for social isolation.
Racial and ethnic minority groups, particularly Black Americans, are more susceptible to many of the top chronic health conditions in the United States, including heart disease, stroke, diabetes, and Alzheimer’s disease. Additionally, differences in prevalence and risk of experiencing childhood trauma and abuse exist across racial and ethnic groups. Though some studies have found that whites are more likely to report ACEs and have higher ACE scores, other studies have shown that there are particular adversities that racial and ethnic minority groups are more likely to experience, and Black American children, along with Hispanic children, were exposed to ACEs more often than non-Hispanic white children (Gilbert et al., 2015; Slopen et al., 2016). For example, Black Americans are more likely than whites to report experiencing physical neglect in childhood (Mersky and Janczewski, 2018), which may provide a negative depiction of family caregiving. This may influence how Black American families approach caregiving in later life.
Caring for someone with Alzheimer’s disease can quickly become intensive as the condition progresses, and caregivers without adequate resources and support can gradually become disconnected from their social network and communities. Caregiving tasks for this health condition require extensive monitoring, engagement, and hands-on care. Twenty six percent of caregivers reported caring for someone with Alzheimer’s disease, and 11 percent report Alzheimer’s disease as the primary health condition of their care receiver (AARP and National Alliance for Caregiving, 2020). Black Americans are more likely to be caring for someone with multiple medical problems, including Alzheimer’s disease. Some research has shown that the prevalence and risk of Alzheimer’s disease is disproportionately higher among Black Americans. It is not unreasonable to conclude that cumulative disadvantages may place Black American caregivers and the older adults that they care for at higher risk for social isolation because of greater rates of emotional ACEs and physical disorders (Alzheimer’s disease, chronic health problems). Moreover, these caregivers may have a history of ACEs and negative perceptions of caregiving, which place the care receiver at risk for abuse and neglect.
Risk and Protective Factors for Black American Caregivers
Based on research findings, one could hypothesize that the disadvantages faced by Black American caregivers and those for whom they provide care would place them at higher risk for social isolation. But research on burden and stress among this population has shown lower risk for emotional distress. Specifically, Black American caregivers consistently report lower levels of burden and emotional stress. This is surprising, given that Black American caregivers disproportionately provide more care for older adults with complex needs than other caregivers.
Caregiving tasks for someone who has Alzheimer’s require extensive monitoring, engagement, and hands-on care.
They are more likely than other racial and ethnic groups to be providing high-intensity care for recipients who have multiple chronic conditions, averaging more than thirty-one hours per week of care of care for people with at least two chronic conditions. Sixty-seven percent of Black American caregivers assist with medical and nursing tasks. They are also more likely to live with their care receivers and provide help with more than just traditional activities of daily living (ADL) and instrumental activities of daily living (IADL). In addition to ADLs and IADLs, Black American caregivers communicate with healthcare professionals and advocate for their loved ones. Compared to other racial groups, Black American caregivers are more likely to be working while providing care and face higher financial burdens as a result of providing care.
Black American caregivers are also more likely to have chronic health conditions, and less likely to report good or excellent health compared to other groups. Social support and social connection may be buffer between higher caregiving and lower burden among Black American caregivers. The presence of social support indicates a lower risk for social isolation.
Given the high-risk indicators in this population of family caregivers, research on social isolation should be a high priority. However, there is paucity of research on social isolation among Black American caregivers. Two demographic studies looked at racial differences in relation to social isolation among community-living older adults. One found that older Black American adults are less likely to experience social isolation compared to whites (Cudjoe et al., 2018). But another earlier study found that older Black Americans are the most likely to be socially isolated compared to other racial and ethnic groups (Locher et al., 2005). So, the findings are inconclusive about social isolation in this community.
An interesting question: are Black American caregivers to older adults at a lower risk or higher risk for isolation, given the higher rates for complex caregiving? Also, what influence does early life trauma have on social isolation and which variables serve as buffers against social isolation in this population?
Our model, the Caregiver-ACE Family Systems Model of Risk and Protection for Social Isolation, was adapted from the National Academies of Sciences, Engineering and Medicine’s (2020) guiding framework of social isolation. The original framework shows the complex relationships among different variables and social isolation risk. Our model presents in greater detail the risk and protective factors for social isolation, as well as incorporating ACEs and race and ethnicity.
Figure 1 (below) shows that early life factors, such as ACEs, familial values and customs, and childhood living arrangements can directly and indirectly influence other factors that increase or decrease the risk for social isolation. For example, people who grow up in a multigenerational household may have had more social support and resources and may be more likely to maintain connections with family throughout their lives, thus lowering the likelihood of social isolation. On the other hand, someone who lived in a multigenerational household during childhood also may have been more likely to experience ACEs, leading to negative health outcomes and fragmented familial relationships, thus increasing the risk of social isolation.
Figure 1. Caregiver-ACE Family Systems Model of Risk and Protection for Social Isolation
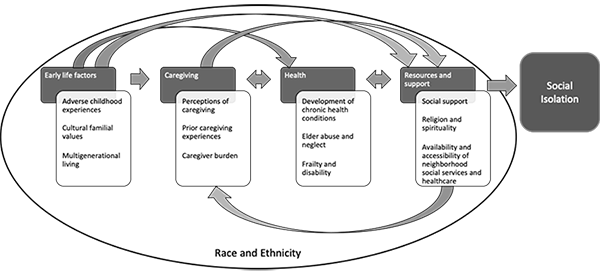
Race and ethnicity can vary the effects of these factors. Cumulative disadvantage from the effects of systemic racism and discrimination can put Black Americans, particularly, at higher risk of experiencing the negative aspects of these factors, ultimately placing them at higher risk for social isolation. The purpose of our model is to show that though the known risk and protective factors of social isolation are interrelated and bidirectional, they all can begin early in life.
This article highlights the disparities in ACEs among Black American families because it is important to expand research focus on the risk and protective factors that influence social isolation to include early life experiences. Interpersonal and familial experiences in childhood can contribute to the onset and progression of poor health, which, combined with a lack of access to resources, could impact the risk of social isolation among caregivers in this population. ACEs could provide an explanation for conflicting research on social isolation among Black Americans.
Culture, Caregiving, and Social Connection
Because Black American caregivers report lower levels of burden and tend to perceive caregiving as rewarding, the restorative nature of caregiving should be highlighted. We know that high burden can lead to strained caregiving relationships, especially if there have been unresolved grievances. Yet, caregiving may be an opportunity to restore relationships and build healthier connections. Caregiving can bring about feelings of gratefulness and appreciation, especially when time with the care receiver is limited.
There are other protective factors that are more prevalent among Black Americans. Black American families are more likely to engage in multigenerational living and report higher levels of religiosity and spirituality, and more connections to their social networks both inside and outside the home. Multigenerational living can allow caregivers to delegate caregiving tasks to others in the household and pool together resources. Offloading grocery shopping, cooking, or cleaning may lower the burden for primary caregivers who provide heavy hands-on care, such as toileting and dressing. Multigenerational living also can make respite care easily accessible, as other household members may be able to temporarily take over caregiving tasks for the primary caregiver. Among Black American caregivers who report higher levels of religiosity, the church can be a source of instrumental and social support, especially in neighborhoods that lack healthcare and caregiving resources. Churches often serve as a source of resources and services for the community. Religious caregivers also lean upon religion to develop healthy coping mechanisms when dealing with tension, burden, and conflict in care. Other church members can serve as emotional and instrumental support.
Also, kinship ties are important in Black American families; they heavily rely on relatives and fictive kin for social support, with 20 percent of Black American caregivers reporting that children help with caregiving tasks (AARP and National Alliance for Caregiving, 2020). Knowing that children often share caregiving tasks, it can be assumed that some Black American families are exposed to caregiving in early life, could develop healthy coping strategies, and recognize that social and emotional support is necessary to adequately provide care.
Black Americans also are known to have high resiliency and tend to recover from or cope better with stressors and traumas, such as systemic racism and discrimination. This resilience may apply to ACEs as well. It is plausible that Black American caregivers are able to set aside previous grievances to tend to their relative’s care needs, especially if they have to coordinate and share care tasks with other family members. Religion also may be tied to this resiliency, as people who are religious tend to use their faith to remain optimistic and maintain peaceful interactions and relationships. In caregiving, religious Black American caregivers tend to credit strong faith and perseverance in managing difficult tasks and dealing with interpersonal problems. Rather than using more traditional therapeutic methods to cope, they often turn to church members and leaders.
Black American families are more likely to engage in multigenerational living and report higher levels of religiosity and spirituality.
However, it is possible that ACEs may cause problems in caregiving relationships. Contentious relationships may extend into late life, and ACEs also could prevent restoration of relationships and increase tension and stress, especially if the care receiver was responsible for the ACE traumas. In caregiving relationships where the care receiver has Alzheimer’s disease, there is likely to be high intensity caregiving tasks and a higher burden among caregivers. Additionally, tension and conflict likely will arise, often due to behavioral issues of the care receiver, and ACEs can exacerbate conflict. ACEs can be additive, as already highly burdened caregivers would also have to cope with past trauma. In families where one or more members have high ACEs, collaborative and coordinated care can bring about discord among family members resulting in fragmented and inadequate care of the older adult, unhealthy coping strategies, and the caregiver reducing or discontinuing interactions with family members.
Recommendations
Practitioners should not only focus on problems that need to be fixed, but also, they need to think about building upon the strengths in caregiving families. Practitioners also should consider training more healthcare professionals and service providers who serve and interact with caregivers on trauma-informed care. It is important to produce empirical data on ACEs and their impacts on caregiving relationships later in life, as well as their possible impact on social isolation risk. Continuing research on racial and ethnic differences in the risk for social isolation will help to create a cohesive body of literature for practitioners.
California has enacted policy efforts to reduce ACEs and buffer negative health outcomes by training physicians to screen for and address ACEs in patients. Collecting ACE data more often from caregivers and older adults could help to better screen for risk of several late-life conditions and circumstances, including social isolation. Although researchers tend to focus on health outcomes as a result of high ACEs, they also should focus on how ACEs impact familial relationships over the life course.
Incorporating early life experiences can give practitioners a better understanding of the mechanisms and pathways to social isolation not only for Black American families but also for all caregiving families. The authors challenge practitioners, clinicians, and academics in gerontology to consider early life trauma and abuse when tackling interventions and prevention of social isolation. Moreover, it is important to consider how to incorporate the strengths that reduce burden and stress among Black American caregivers to older adults into interventions for family caregivers.
Donna Benton, Ph.D., is the director of the Los Angeles Caregiver Resource Center and a research associate professor at the Leonard Davis School of Gerontology, University of Southern California, in Los Angeles, CA. She can be contacted at benton@usc.edu. Elizabeth S. Avent, M.A., is a doctoral candidate at the Leonard Davis School of Gerontology, University of Southern California, in Los Angeles, CA. She can be contacted at eavent@usc.edu.
References
AARP and National Alliance for Caregiving. 2020. Caregiving in the United States 2020. Washington, DC: AARP.
Anda, R. F., et al. 2008. “Adverse Childhood Experiences and Chronic Obstructive Pulmonary Disease in Adults.” American Journal of Preventive Medicine 34(5): 396-403.
Brown, M. J., Thacker, L. R., and Cohen, S. A. 2013. “Association Between Adverse Childhood Experiences and Diagnosis of Cancer.” PLOS ONE 8(6): e65524.
Center for Youth Wellness and Public Health Institute. 2014. “A Hidden Crisis: Findings on Adverse Childhood Experiences in California.” San Francisco, CA: Center for Youth Wellness.
Corso, P. S., et al. 2008. “Health-related Quality of Life Among Adults Who Experienced Maltreatment During Childhood.” American Journal of Public Health 98(6): 1094-100.
Cudjoe, T. K. M., et al. 2018. “The Epidemiology of Social Isolation: National Health and Aging Trends Study.” The Journals of Gerontology: Series B: Psychological Sciences and Social Sciences 75(1): 107-13.
Dong, M., et al. 2004. “Insights Into Causal Pathways for Ischemic Heart Disease.” Circulation 110(13): 1761-6.
Felitti, V. J., et al. 1998. “Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study.” American Journal of Preventive Medicine 14(4): 245-58.
Frank, D. 2018. “Social Isolation: Symptoms, Prevention, Treatments.” Retrieved June 4, 2020.
Gilbert, L. K., et al. 2015. “Childhood Adversity and Adult Chronic Disease: An Update from Ten States and the District of Columbia, 2010.” American Journal of Preventive Medicine 48(3): 345-9.
Locher, J. L., et al. 2005. “Social Isolation, Support, and Capital and Nutritional Risk in an Older Sample: Ethnic and Gender Differences.” Social Science & Medicine 60(4): 747-61.
Merrick, M. T., et al. 2018. “Prevalence of Adverse Childhood Experiences from the 2011-2014 Behavioral Risk Factor Surveillance System in 23 States.” JAMA Pediatrics 172(11): 1038-44.
Mersky, J. P., and Janczewski, C. E. 2018. “Racial and Ethnic Differences in the Prevalence of Adverse Childhood Experiences: Findings from a Low-income Sample of U.S. Women.” Child Abuse & Neglect. 76(February 2018): 480-7.
Morin, A. 2018. “Loneliness Is as Lethal As Smoking 15 Cigarettes Per Day. Here’s What You Can Do About It.” Inc. Retrieved June 4, 2020.
National Academies of Sciences, Engineering, and Medicine. 2020. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. Washington, DC: The National Academies Press.
Slopen, N., et al. 2016. “Racial Disparities in Child Adversity in the U.S.: Interactions with Family Immigration History and Income.” American Journal of Preventive Medicine 50(1): 47-56.
Tani, Y., Fujiwara, T., and Kondo, K. 2020. “Association Between Adverse Childhood Experiences and Dementia in Older Japanese Adults.” JAMA Network Open 3(2): e1920740-e1920740.













