Incentivizing Americans to make healthy lifestyle choices has been part of the Centers for Medicare & Medicaid Services (CMS) Administrator Dr. Mehmet Oz’s vision for improving U.S. healthcare since he first articulated it in the opening statement of his March 2025 Senate confirmation hearing.
Aligned with this in May, the CMS Center for Medicare & Medicaid Innovation (CMMI) announced its priorities would include empowering people to drive and achieve their own health goals, via a focus on evidence-based prevention interventions like physical activity and good nutrition. Fast forward to January 2026, and we already see new CMMI models incorporating nutrition.
| What is CMMI? The Center for Medicare & Medicaid Innovation (CMMI)—often called the Innovation Center—is a division of the Centers for Medicare & Medicaid Services (CMS) created under the Affordable Care Act. Its mission is to test new payment and service delivery models that aim to reduce healthcare costs while preserving or improving quality of care for people enrolled in Medicare, Medicaid and CHIP. Rather than making permanent changes immediately, CMMI pilots time-limited, data-driven models. If a model successfully improves quality and lowers costs, CMS has the authority to scale it nationally without additional Congressional action, discontinue the model, or replace the model with refined focus for better outcomes. |
CMMI models present opportunities to improve nutrition and health outcomes for an aging population because the models frequently focus on recipients with high-risk, high-cost, and complex-needs—including many older adults with chronic conditions who can be at risk for poor nutrition. This blog post identifies CMMI models where nutrition is incentivized and/or specifically included.
CMMI Strategy to Make America Healthy Again
CMMI introduced the Innovation Center’s Strategy to Make America Healthy Again in May 2025, outlining their vision to use what is learned and build a health system, “that empowers people to drive and achieve their own health goals.” This vision encompasses various age groups (including those aging into Medicare and those ages 80 and older), populations, geographies and those with special needs or disabilities. To see this vision to fruition, CMMI designated three pillars as guidance for their future evidence-based programs:
- Promote evidence-based prevention
- Empower people to achieve their health goals
- Drive choice and competition for people.
The three pillars guide how CMMI models are designated and evaluated. CMMI models are intended to move the health system away from volume‑based care and toward value‑based care, where payment is tied to outcomes, prevention, and long‑term health improvements rather than the number of services delivered. Many models seek to improve access for underserved populations/providers, including rural communities, people with complex or chronic conditions, and safety-net providers. This includes expanding access to non‑traditional services, such as nutrition education and lifestyle support programs, based on evidence suggesting improved outcomes that align with the three pillars.
CMMI Models Incentivizing and/or Including Nutrition
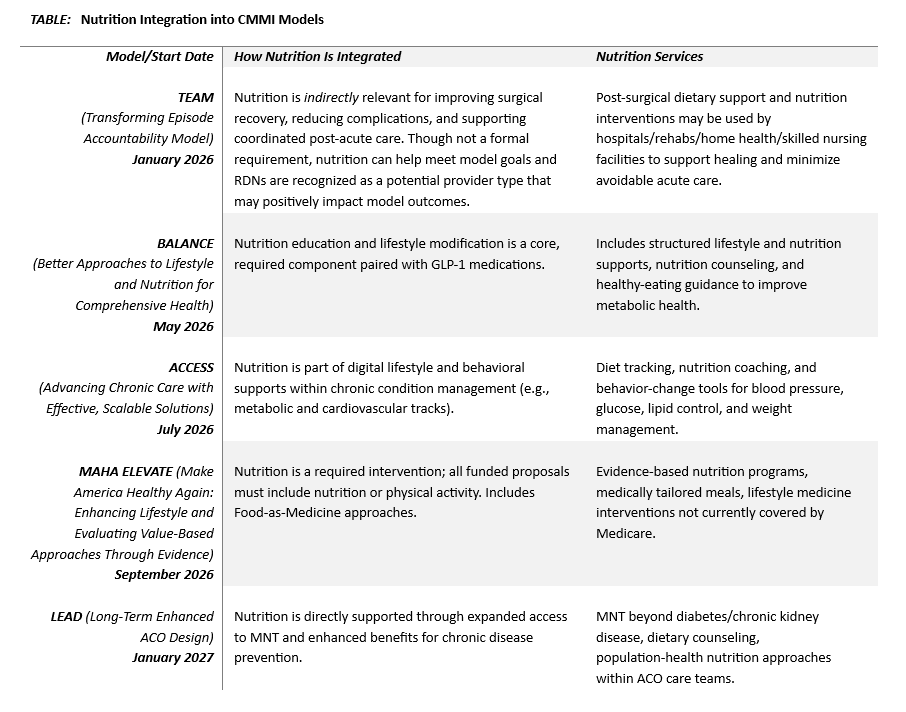
Some CMMI models have included a component related to nutrition, such as the Medicare Diabetes Prevention Program (MDPP) that focuses on preventing type 2 diabetes through behavior changes (diet and exercise). In contrast, five new CMMI models are increasingly integrating nutrition as a core part of preventive care and chronic disease management, as described below. The Table summarizes how each of the five CMMI models integrates nutrition—directly, indirectly, or as part of broader whole‑person care.
TEAM Model: Transforming Episode Accountability Model
Although the TEAM model does not explicitly require nutrition interventions, its structure creates strong incentives for hospitals and care partners to incorporate nutrition into perioperative and post‑acute management by engaging with providers known as “TEAM collaborators.” These providers can impact a TEAM participant’s performance in the model.
CMS explicitly recognized Registered Dietitian Nutritionists (RDNs) as possible TEAM collaborators that model how participants may wish to engage to ensure they achieve positive outcomes. TEAM addresses fragmented care following major surgeries, aiming to reduce complications and readmissions through improved coordination across the 30‑day episode.
Post‑surgical recovery is strongly influenced by nutrition status—adequate protein, energy intake, and micronutrients can reduce infection risk and support improved healing. TEAM’s accountability for outcomes encourages hospitals and skilled nursing facilities to incorporate nutrition assessments and interventions to minimize costly readmissions or prolonged recovery. While indirect, nutrition becomes an important lever for achieving the model’s goals of reduced acute care use and risk of readmissions after surgery.
BALANCE Model: Better Approaches to Lifestyle and Nutrition for Comprehensive Health
Nutrition is at the center of the BALANCE model. Designed to expand access to GLP‑1 medications for metabolic conditions, BALANCE explicitly pairs medication therapy with lifestyle and nutrition‑based supports. Through the model, CMS negotiates pricing with GLP‑1 manufacturers and requires participating entities to provide evidence‑based nutrition support alongside medication.
ACCESS Model: Advancing Chronic Care with Effective, Scalable Solutions
The ACCESS model expands technology‑supported care for chronic conditions and uses outcome‑aligned payments to reward clinical improvements. While nutrition is not the sole focus, it is embedded as a major lifestyle and behavioral support, especially in cardiovascular and metabolic care tracks.
MAHA ELEVATE Model: Make America Health Again: Enhancing Lifestyle and Evaluating Value-Based Approaches Through Evidence
MAHA ELEVATE focuses on whole-person functional and lifestyle medicine, specifically including nutrition, physical activity, and related behavior-change strategies. It supports interventions such as nutrition programs, food is medicine, stress management and harmful substance avoidance. The cooperative agreements that are awarded funding are specifically challenged to include services not already covered by the original Medicare program.
This creates an avenue for Medical Nutrition Therapy (MNT) to be provided beyond current Medicare MNT coverage (limited to patients with diabetes and/or renal disease), potentially benefiting Medicare patients with other chronic diseases such as obesity, malnutrition, cancer, and cardiovascular disease. MNT is individualized nutrition intervention provided by an RDN to treat or manage medical conditions and diseases. The Academy of Nutrition and Dietetics recently stated that food as medicine programs provided simultaneously with MNT elevate the significance of nutrition in health outcomes.
LEAD Model—Long‑term Enhanced Accountable care organization (ACO) Design
A successor to the ACO REACH model, the LEAD model represents CMMI’s longest ACO test model, running from 2027 to 2036. LEAD includes expanded benefit enhancements that allow participating ACOs to invest more flexibly in nutrition counseling, MNT, and food‑related supports, especially for beneficiaries with chronic disease conditions such as pre-diabetes or hyperlipidemia. Nutrition is already positioned as a foundational element of preventive care and healthy aging within accountable care structures, creating increased opportunities for RDNs to play an integral role in preventive services, interdisciplinary care teams, and community-based supports.
Nutrition-Focused Opportunities Ahead
Across the new CMMI models identified, the Agency is signaling a critical and consistent shift: nutrition is no longer peripheral. While some CMMI models (TEAM) address nutrition indirectly, others—BALANCE, MAHA ELEVATE, ACCESS, and LEAD—explicitly recognize nutrition as a clinical, preventive, and cost‑saving intervention. Together, these models illustrate how CMMI is testing ways to embed nutrition into payment design, care delivery, and long‑term health outcomes, which will promote healthy aging and better support older adults and their families.
Amy Shepps, MBA, RDN, is the director of corporate reimbursement for Abbott in Washington, DC. Kimberly Iles, MS, RDN, is the senior manager of nutrition services coverage at the Academy of Nutrition and Dietetics in Chicago, Ill.
Photo credit: Creation Company













