Abstract
As the older population grows, elder care demand increases, putting significant pressure on professional caregivers and family members. Caregivers often face emotional and physical strain, while older people risk social isolation and delayed medical intervention. Technology is transforming the landscape of elder care by streamlining health monitoring, improving decision-making, and fostering meaningful connections. By integrating advanced tools such as smart sensors, AI-driven analytics, and automated communication systems, we can create a caregiving environment that is efficient and compassionate—one that reduces burnout and prioritizes physical and emotional well-being.
Key Words
wearable technologies, sensing, smart technologies, internet of things (IoT), vital signs, personalized healthcare, personal digital assistant (PDA)
Traditionally, older individuals receive medical attention during scheduled clinic visits, which can miss subtle but important health changes. Continuous health monitoring fills this gap to enable earlier intervention and improved care management via real-time insights.
Increasingly, physiological and behavioral patterns can be continuously monitored in real time, enabled by diverse sensing modalities, ranging from wearable devices to environmental sensors deployed in smart homes and buildings. These technologies facilitate the capture of granular data related to activity, sleep, vital signs, and even subtle changes in environmental factors that affect well-being. The resultant streams of data offer an opportunity to move beyond episodic assessments toward proactive and personalized health management, as well as a deeper understanding of individual and population health trends.
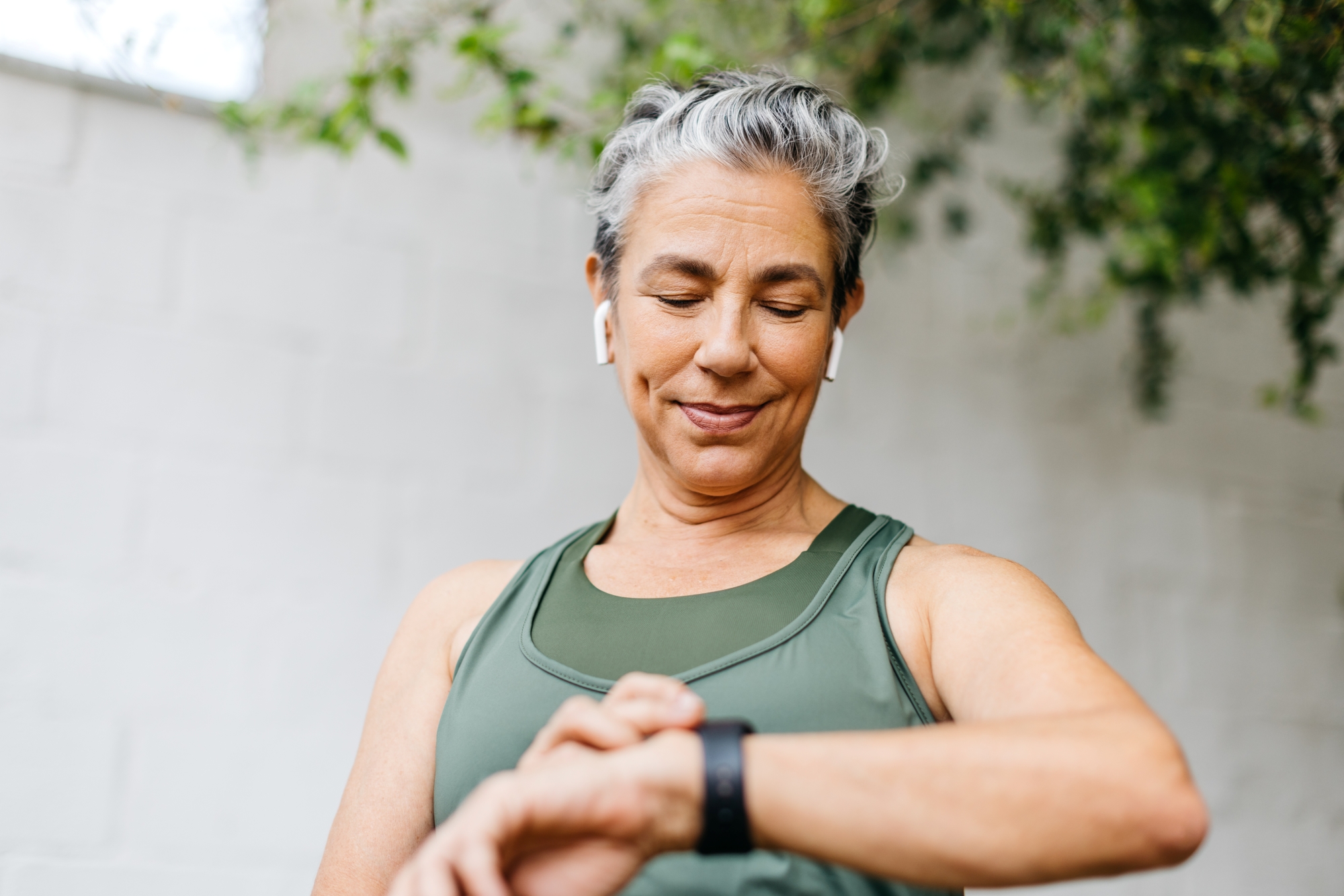
Real-Time Health Tracking Using Wearables
Wearable devices have revolutionized elder care by providing round-the-clock monitoring of key health indicators. These include smartwatches that can detect falls in addition to tracking heart rate, breathing rate, and oxygen levels. In addition, advances in materials have made adhesive patches accessible and able to report physiological requirements with finer resolution, such as electrocardiogram (ECG) signals, hydration, blood-sugar levels, and temperature fluctuations (Hussain et al., 2023).
Biometric sensors can be embedded in clothing to track posture, mobility, and various signs of distress such as irregular heartbeats or breathing patterns (Kang et al., 2006). Wearable technologies coupled with AI can be tuned to be highly specific, resulting in a high degree of personalization.
Studies analyzing individual breathing patterns can reveal changes from baseline, suggesting onset of illness (Wajid et al., 2024). And wireless sensing can be deployed to not only measure vital signs, but also to recognize emotions (Zhao et al., 2016). By reducing the need for constant monitoring, such wearables can alleviate caregiver workload while enhancing older adults’ safety and independence.
Enhancing Emotional Well-Being Through Technology
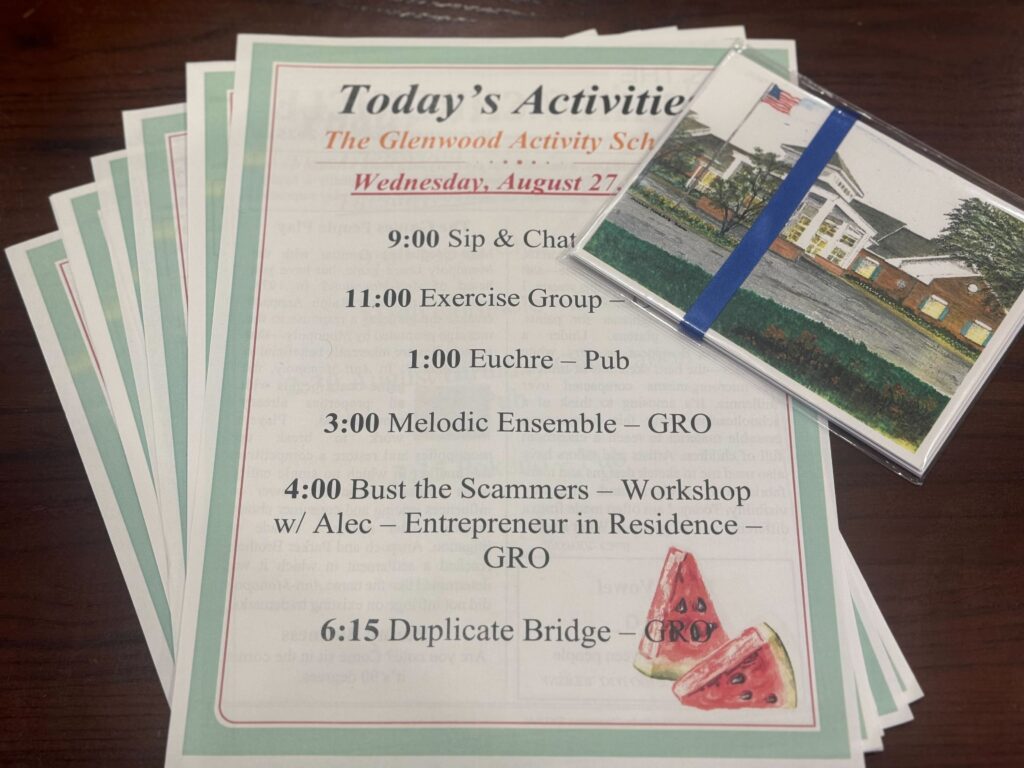
While physical health is a priority, emotional well-being is equally vital in elder care. Many older adults experience loneliness and social isolation, which are linked to increased risks of depression, cognitive decline, and even mortality. Technology offers innovative ways to foster social engagement, emotional resilience, and a sense of belonging.
‘Wireless sensing can be deployed to not only measure vital signs, but also to recognize emotions.’
In addition to video calls and messaging platforms, AI companionship devices—ranging from voice assistants to socially responsive robots—offer interactive conversations, reminders, and games that provide comfort and reduce feelings of isolation. Augmented and virtual reality (AR/VR) systems present promising avenues for immersive engagement. Older adults can participate in virtual group activities, revisit familiar or meaningful locations through 360-degree video environments, or engage in mindfulness exercises—all from the safety of their residence. These virtual experiences have been shown to reduce anxiety and improve mood, while also helping users feel more connected to broader communities (Yang et al., 2025).
Mood- and behavior-tracking technologies also support caregivers by flagging early signs of emotional distress, enabling timely interventions. By offloading routine tasks, technology frees caregivers to focus on building meaningful human relationships, ultimately supporting the emotional well-being of both older adults and those who care for them. These technologies provide comfort and cognitive stimulation, particularly for those living alone or in understaffed facilities.
Smart Homes vs. Assisted Living for Environmental Monitoring
Beyond wearable technology, smart environments play a crucial role in supporting independent and assisted living settings. Pervasive sensing through outfitting residential homes and/or assisted living facilities shows promise in enhancing resident wellness.
Smart Homes: Enhancing Safety and Independence
For older adults living at home, smart technologies provide a safety net, ensuring their well-being without requiring constant supervision. Smart home technologies have the capacity to transform how older people can safely age in place while promoting autonomy and ensuring timely interventions as appropriate. Integrating motion sensors and fall-detection systems can identify prolonged inactivity or abrupt movements, automatically triggering alerts to caregivers or emergency services (Greene et al., 2016).
Already, voice-activated home assistants can remind users to take medications, drink water, attend appointments, or perform physical activities, reducing reliance on memory and routine-based caregiving. One can augment these sensing modalities with environmental sensors that continuously monitor indoor air quality, humidity, and temperature to adjust climate conditions and comfort (Thermal Environmental Conditions for Human Occupancy, 2023), or issue warnings when thresholds fall outside safe ranges (Schieweck et al., 2018). These intelligent systems not only provide critical oversight without intruding on personal space but also offer a layer of reassurance to caregivers. The resulting environment is one in which older adults can retain dignity and independence while benefiting from an infrastructure geared toward safety, which adapts to their needs in real time.
Assisted Living Facilities: Smarter Care Coordination
In modern assisted living environments, technology is redefining how care is delivered, enabling staff to provide responsive support while preserving the dignity and autonomy of residents. AI-assisted camera systems now offer real-time monitoring that can detect signs of distress, wandering, or sudden health changes, all while maintaining residents’ privacy through selective data processing and non-invasive observation techniques (Ravi et al., 2024). Automated diagnostic stations can perform routine health evaluations, such as blood pressure or temperature checks, streamlining workflows and allowing clinical staff to focus on higher-priority tasks or personalized engagement.
‘Technology reinforces a care environment that is proactive, not reactive, ensuring health challenges are met with speed, structure, and compassion.’
By embedding intelligent systems into facility operations, assisted living centers can enhance care quality and reduce response times and staff workload, all aimed at optimizing staff efficiency, while ensuring that every resident receives timely and appropriate attention.
Action Initiation: Timely and Organized Response
Detection alone is not enough: Intervention must be swift, coordinated, and appropriate to the severity of the situation. Here the success metric is how well issues are identified, and a proportionate response is carried out given the situation. Intelligent systems should be developed with care to facilitate immediate action across relevant parties, ensuring that older individuals receive prompt care and support.
Smarter Decision-Making
The vast amount of health data collected from wearable devices and smart environments presents a dual challenge: Is it possible to extract valuable insights without overwhelming caregivers? AI must play a pivotal role in filtering, analyzing, and contextualizing these data streams. Continuous monitoring is valuable in determining patient baselines for normality, and when modeled in conjunction with advanced algorithms, can identify subtle patterns to isolate anomalous signals that could indicate warning signs of health deterioration (Ting et al., 2025).
Furthermore, prioritization systems that categorize alerts based on urgency will allow care teams to focus on critical situations without succumbing to alarm fatigue. This data-driven approach empowers caregivers to act with greater precision and confidence, ultimately leading to more proactive interventions, improved outcomes, and reduced burden on healthcare personnel.
Smart Notification Systems
Automated alert systems would act as central nodes in the caregiving network in efforts to streamline communication and direct attention to where it is needed most. These systems will be designed to prioritize alerts based on severity: Professional caregivers would be instantly notified of high-risk health events such as falls or cardiac irregularities, enabling rapid medical response. Non-emergency notifications such as skipped meals or decreased mobility could be routed to family members or designated contacts, encouraging timely yet non-intrusive support. In critical situations, emergency medical services would be automatically notified with relevant medical records and recent sensor data, accelerating diagnosis and treatment enroute or upon arrival.
Enhanced Coordination in Assisted Living and Nursing Homes
By integrating these solutions, older adults can receive faster, more organized responses, while caregivers are empowered to dedicate more time for personal interactions and developing deeper connections with residents. Rather than being overwhelmed by data, caregivers can focus on providing compassionate support, ensuring both the well-being of older adults and their own professional fulfillment.
In care facilities, these systems offer further operational efficiency and clinical effectiveness. Access to real-time dashboards and alerts will ensure that staff are continuously informed of residents’ changing conditions, minimizing the risk of missed early warning signs. Automated emergency protocols will reduce reliance on manual decision-making during crises, decreasing the potential for human error. By offloading routine checks and coordination tasks, caregivers are afforded the time and clarity to focus on empathetic, resident-centered care.
Together, these innovations hold the promise to shift the burden of vigilance from individuals to systems, promoting responsive care and caregiver sustainability. Through organized and intelligent action initiation, technology reinforces a care environment that is proactive, not reactive, ensuring health challenges are met with speed, structure, and compassion.
Conclusion: A Future of Balanced, Tech-Enabled Care
Technology is not here to replace caregivers—it is here to support them. The advancements mentioned above grant us tools and approaches to reduce clinical burden and caregiver burnout by automating routine tasks, providing real-time health insights, and fostering social connections. This allows caregivers to focus on what’s most important: improving the overall well-being of older adults.
With these advancements, older adults can enjoy safer, more independent lives, while caregivers—professional and family—can experience greater peace of mind and a renewed focus on compassionate, meaningful interactions. As we move forward, the integration of these innovations will shape a future where elder care is not only more efficient but also more humane, ensuring dignity, comfort, and connection for all.
Mara Cai is the chief research scientist of the MIND Lab at the University of Maryland, dedicated to building intelligent systems that enhance human well-being and quality of life. Her work focuses on bridging technology and holistic understanding of systems to create tools that empower individuals and communities. Ashok Agrawala, PhD, is a professor in the University of Maryland Department of Computer Science and director of the MIND Lab. His work focuses on context-aware pervasive systems and wearable/sensing technologies. His past work includes developing a real-time location tracking app called Locus, co-developing the Ricart-Agrawala Algorithm, and leading the field with numerous publications.
Photo credit: Shutterstock/JLco Julia Amaral
References
Greene, S., Thapliyal, H., & Carpenter, D. (2016). IoT-based fall detection for smart home environments. In 2016 IEEE International Symposium on Nanoelectronic and Information Systems (iNIS). IEEE. https://doi.org/10.1109/iNIS.2016.017
Hussain, T., Ullah, S., Fernández-García, R., & Gil, I. (2023). Wearable sensors for respiration monitoring: A review. Sensors, 23(17), 7518. https://www.mdpi.com/1424-8220/23/17/7518
Kang, T. H., Merritt, C., Karaguzel, B. Wilson, J., Franzon, P. Pourdeyhimi, B., Grant, E. & Nagle, T. (2006). Sensors on textile substrates for home-based healthcare monitoring. In Proceedings of the 1st Transdisciplinary Conference on Distributed Diagnosis and Home Healthcare, D2H2 (pp. 5–7). IEEE. https://doi.org/10.1109/DDHH.2006.1624783
Ravi, S., Climent-Pérez, P., & Florez-Revuelta, F. (2024). A review on visual privacy preservation techniques for active and assisted living. Multimedia Tools and Applications, 83, 14715–14755.
Schieweck, A., Uhde, E., Salthammer, T., Salthammer, L. C., Morawska, L., Mazaheri, M., & Kumar, P. (2018). Smart homes and the control of indoor air quality. Renewable and Sustainable Energy Reviews, 94, 705–718. http://dx.doi.org/10.1016/j.rser.2018.05.057
Thermal Environmental Conditions for Human Occupancy. (2023). ANSI/ASHRAE Standard 55-2023.
Ting, L. P. Y., Chen, H. P., Liu, A. S., Yeh, C. Y., Chen, P. L., & Chuang, K. T. (2025). Early detection of patient deterioration from real-time wearable monitoring system [arXiv preprint 2505.01305]. arXiv . https://doi.org/10.48550/arXiv.2505.01305
Wajid, F., Cai, M., & Agrawala, A. (2024). Anemoi: Breath analytics for ailment prediction and recovery tracking [Conference paper]. EAI Endorsed Transactions on Pervasive Health and Technology. https://pervasivehealth.eai-conferences.org/2024/accepted-papers/
Yang, Y., Wang, C., Xiang, X., & An, R. (2025). AI applications to reduce loneliness among older adults: A systematic review of effectiveness and technologies. Healthcare (Basel), 13(5), 446. https://doi.org/10.3390/healthcare13050446
Zhao, M., Adib, F., & Katabi, D. (2016). Emotion recognition using wireless signals. In Proceedings of the 22nd Annual International Conference on Mobile Computing and Networking (pp. 95–108). Association for Computing Machinery Press. https://dspace.mit.edu/handle/1721.1/112922