Editor’s note: The John A. Hartford Foundation, the Administration for Community Living (ACL) and The SCAN Foundation fund the Aging and Disability Business Institute, led by USAging. The mission of the Aging and Disability Business Institute is to build and strengthen partnerships between aging and disability community-based organizations (CBO) and the healthcare system. As partners in the Institute, ASA and USAging are collaborating on a series of articles and case studies in Generations Today that spotlight the 2021 winners and runners up for The John A. Hartford Foundation Business Innovation Award.
DayBreak Adult Care Centers is headquartered in San Leandro, a relatively quiet suburb of Oakland, Calif., and serves older adults and their family caregivers across Alameda County. DayBreak is this year’s runner up for The John A. Hartford Foundation’s Business Innovation Award.
Most clients at DayBreak have severe physical and memory impairment challenges, and the agency has a robust family caregiver support arm as well as a care coordination arm, according to Ofra Paz, its executive director. DayBreak also provides injury prevention programming with exercise classes and home modifications and a program for medication management.
In 2018, DayBreak started a Rapid Response Case Management Pilot, which came about out of what Paz calls a “huge failure,” thus proving that adage about failure being the mother of innovation. Alameda County Emergency Medical Services (EMS) had reached out to all organizations in the county with senior injury prevention programs, to put in place more upstream falls prevention, which would cut down on older adults dialing 911 for falls and injuries. DayBreak started meeting with EMS and a group of community-based organizations (CBOs) to which EMS could refer such older adults.
The first step was to embed the CDC’s STEADI (Stopping Elderly Accidents, Deaths & Injuries) program for assessing falls risk into the Emergency Medical Technician (EMT) protocol. That way if a person had been identified as a high falls risk, they could be referred to a CBO in the pilot program for help in preventing future falls and injuries. The only snag (failure) with this original setup was that EMTs are not in the habit of gathering phone numbers, so there was no way to reach the clients after the fact.
But all was not lost as DayBreak had access to the 911 call data. “Imagine what we found,” said Paz. There was a wealth of information available and as Paz said, “the intervention just jumped out of the data.”
Older adults in Alameda County account for more than 40 percent of 911 calls, but only 15 percent of the population.
DayBreak now knew where and why people were calling, how many times they called and to which hospital they were taken. Paz said they figured they needed to meet the person in the middle of the crisis and work with them from there. With the help of EMS, they identified a hospital in the county to work with. There was strong buy-in from the care coordination manager who understood what they were aiming to do, and they received a small seed grant of $20,000 from the Kaiser Community Benefit to start the pilot.
Evolving and Paying for the Pilot
Older adults in Alameda County account for more than 40 percent of 911 calls, said Paz, which is extraordinary considering they make up about 15 percent of the population. High-frequency older adult users tend to call six or more times per year. “We were seeing how this small group of people were keeping the system so busy in a crazy way,” said Paz.
Her organization, in partnership with EMS and other CBOs, analyzed the reasons and isolation rose to the top of the list. “Really what drives this behavior, which is sometimes a compulsive behavior,” said Paz, “is that it’s caused by behavioral health issues or by people who are isolated or lonely. The only place they know they can call and get an answer is 911. 911 always answers, and they always come quicky,” Paz added.
DayBreak figured if this was the problem, why shouldn’t they respond instead of EMTs? People clearly need a rapid response in times of crisis, so why not meet the clients where they are in the community, which would be far less expensive. “It’s not sophisticated, we know how to identify the people (from the data), and work with the systems they are encountering time and again. We also know how to form a partnership [with healthcare entities and CBOs] and build a comprehensive approach to deal with the complexities encountered by our clients,” said Paz.
After six months of the pilot, DayBreak secured $1.5 million to get them through the next five years via a grant for transitional housing for older adult crime victims from the California Office of Emergency Services. It also continues to receive support from other foundations and county funding to augment this budget.
The funding allowed the organization to expand from one case manager to five and from working with one hospital to two. DayBreak also began working with local fire departments to take on their high-end users in addition to those from EMS. And during the pandemic they started working with Adult Protective Services, responding to direct referrals for clients that need intensive support.
‘Partner! You do not do this work on your own, this is not your show to run.’
In the pilot’s first year, 56 percent of DayBreak clients were unhoused or at high-risk of homelessness, plus they had substance abuse and mental health issues. To address this issue, DayBreak developed its own housing solution with supportive independent living. Case managers place people in existing group homes and DayBreak partners with the home’s owners, so clients are not just getting a roof over their heads, but also case managers are working intensely to keep them happily housed.
Care managers refer people to substance abuse help, too, as well as assisting with paperwork, transport to physician appointments, attending physician appointments and helping with communication while there, and medication management. DayBreak provides housing assistance, personal care and any other support to ensure the client is stabilized and has all the support systems in place.
Can the Model Be Replicated?
Although DayBreak’s Rapid Response Case Management program is now funded solely by grants, Paz is certain they will evolve away from that model and into contracting with healthcare entities. They’re now assessing who pays for what in the healthcare system, and what individual entities may be looking for, service wise. Paz said they’ve figured out what they’re doing, how to do it, and the timeframe needed, which is 90 days of intensive care followed by less intensive follow-up care and clients “graduating” in about a year’s time.
Then if the client experiences a setback, because of the established trusted relationship, it’s easier to stabilize clients post-setback.
DayBreak is educating itself on the business side and preparing pilots with HMOs that have expressed an interest in its model. “This model can easily be replicated to any other location,” said Paz. “The principles are very simple, there’s really no sophistication to the model, just to the work the case managers do in the field. They are all highly experienced and know how to deal with trauma and behavior management. And they can maneuver systems of care, which is huge,” added Paz.
Paz also had some wise words for other agencies looking to do similar work: “Partner! Partner! You do not do this work on your own, this is not your show to run, it is always bigger than you or your agency, so to be impactful, you must partner,” she said.
“We have two types of clients, case management clients and systems clients. We partner with both, and the same principles apply: meet them where they are, find out their challenges, find out their history, and culture, how to walk beside them and do the work in a gentle way,” said Paz.
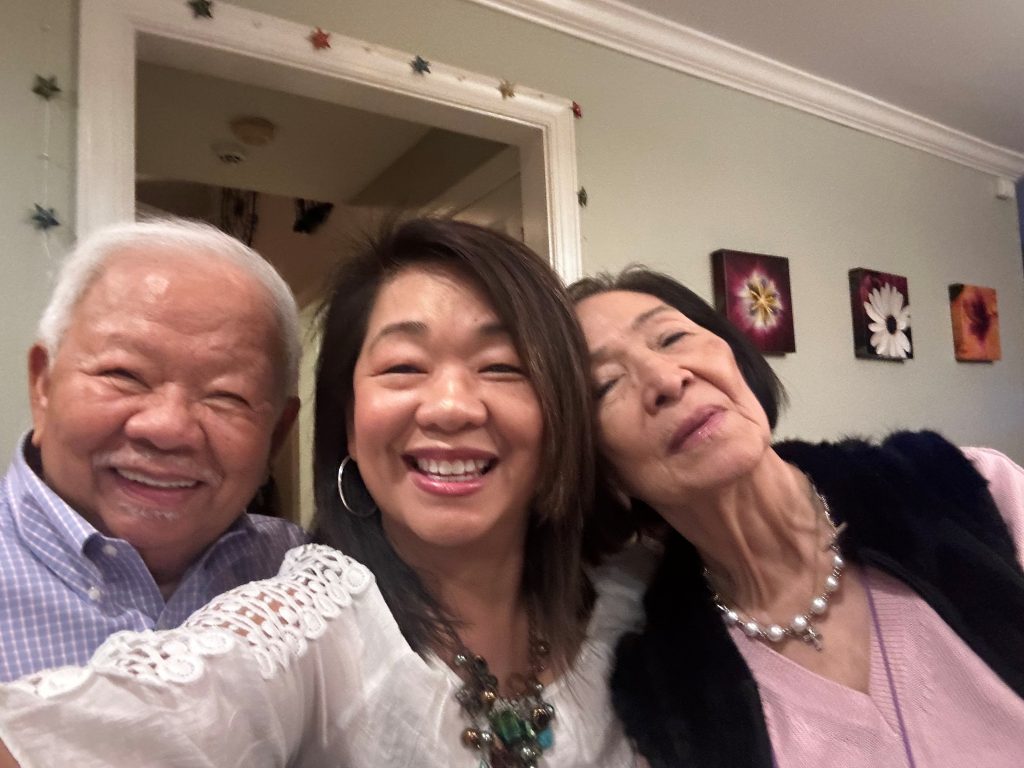
Photo: Stephanie Stevens, DayBreak’s Director of Care Coordination, with a group of clients at one of DayBreak’s Independent Living Home partners.