Almost all Medicare beneficiaries have at least one chronic condition and more than two-thirds live with multiple chronic conditions. What they don’t have is ready access to nutrition care. Studies have shown that Medical Nutrition Therapy (MNT) is a cost-effective service for treating obesity, diabetes, hypertension, dyslipidemia, HIV infection, unintended weight loss and other chronic conditions in older adults. Counseling provided by a registered dietitian nutritionist (RDN) as part of a healthcare team can positively impact weight, blood pressure, blood lipids and blood sugar control.
The Medical Nutrition Therapy Act of 2021 (S. 1536/H.R. 3108) recently introduced by Sens. Susan Collins (R-ME) and Gary Peters (D-MI) and Reps. Robin Kelly (D-IL) and Fred Upton (R-MI) would expand much needed MNT access for Medicare recipients.
Why Expanded Access Is Necessary
According to the CDC, 90 percent of the nation’s $3.8 trillion annual healthcare expenditures is spent on treating individuals with chronic and mental health conditions. Care for individuals with multiple chronic conditions is especially costly in the Medicare population. Yet currently, Medicare Part B only covers outpatient MNT for diabetes, renal disease and post-kidney transplant. While this is important, so many other chronic conditions could benefit from attention to nutrition, too.
In a national survey of primary care physicians, respondents identified RDNs as the most qualified healthcare providers to help patients with weight loss. Also, the National Lipid Association recommends nutritional counseling by RDNs to promote long-term adherence to an individualized, heart-healthy diet.
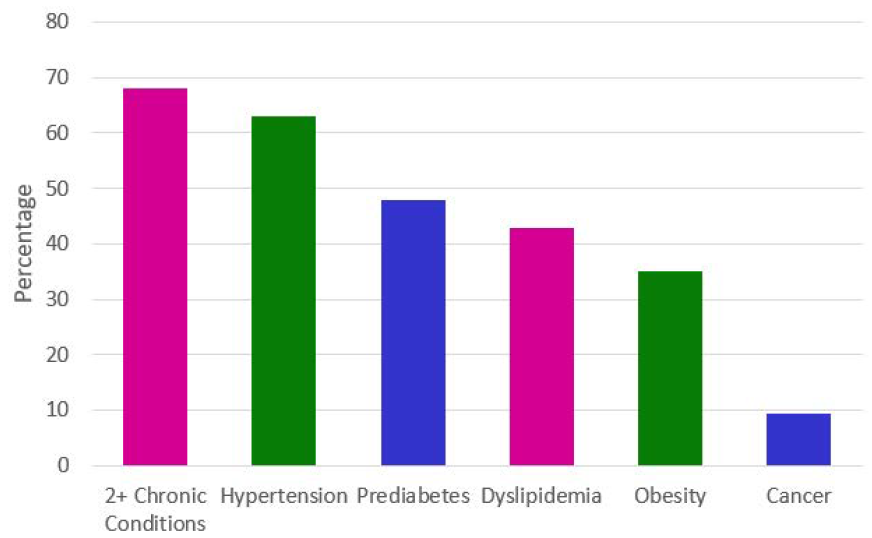
Chronic Disease Burden in Older Adults
The COVID-19 pandemic has highlighted the importance of strong nutrition, and many diet-related chronic conditions were shown to contribute to poor COVID-19 outcomes. Minority populations have long faced chronic disease health disparities due to socioeconomic inequalities and reduced access to healthcare, healthy foods and safe places to be active. It is these same groups that are now disproportionately impacted by COVID-19.
The compounding effects of systemic inequalities, food insecurity, reduced access to care, and now COVID-19, underscore the need to provide equitable access to MNT in Medicare. Also, many Medicare recipients, particularly underserved populations, regularly receive care from nurse practitioners, physician’s assistants, clinical nurse specialists or psychologists. However, these providers are barred from directly referring their patients to MNT services.
What the Medical Nutrition Therapy Act of 2021 Covers
Passage of the MNT Act would significantly expand access to crucial nutrition care services. Here’s what the bill would do:
- Expand Medicare Part B coverage of outpatient MNT to beneficiaries with prediabetes, obesity, high blood pressure, high cholesterol, malnutrition, eating disorders, cancer, gastrointestinal diseases including celiac disease, HIV/AIDS, cardiovascular disease and any other disease or condition causing unintentional weight loss;
- Authorize the Secretary of Health and Human Services to further expand the benefit to other diseases based on clinical guidelines;
- Allow nurse practitioners, physician assistants, clinical nurse specialists and psychologists to refer their patients for MNT; and
- Promote health equity among minority communities with higher rates of nutrition-related chronic diseases.
How You Can Take Action Now to Increase MNT Access and Utilization
The Academy of Nutrition and Dietetics is a proud champion of the Medical Nutrition Therapy Act, which is supported by nearly 50 national organizations. You can add your national organization to the list of supporters here. To give your personal support, visit the Academy’s Action Center and urge your members of Congress to sign on to the Medical Nutrition Therapy Act. You can also promote access to MNT right now, for your patients/clients with diabetes or renal disease. Let these patients know that Medicare fully covers RDN visits with no out-of-pocket costs.
Current referral rates for eligible beneficiaries are unfortunately low and thus there is a great need to educate patients/families and their physicians about this benefit. The Academy has developed resources to help primary care providers partner with and refer to RDNs for improved patient health and well-being.
For more information on the MNT Act, visit the Academy’s MNT Act webpage.
Hannah Martin, MPH, RDN, is a director of Legislative and Government Affairs at the Academy of Nutrition and Dietetics in Washington, DC.